Previously, pathology was considered an ailment of the elderly, the causes of which lay in age-related changes in the bone tissue of the spine. Modern medicine after numerous studies has changed its mind. Now osteochondrosis affects not only patients of retirement age, but is often diagnosed in people under 30 years old. As for the international classification of pathologies, the ICD 10 code for lumbar osteochondrosis is defined as M-42.
CT scan of the lumbar.
The disease proceeds slowly, the symptoms manifest themselves already in the later stages, at the beginning it is quite difficult to suspect such an ailment.
As a rule, the most pronounced clinical picture is noted during the period of exacerbation or when the pathology reaches the second stage. In general, the following symptoms may appear:
- Pain syndrome in the lumbar region during physical exertion. At the beginning, it is noticeable only after lifting heavy objects or playing sports. As it progresses, it becomes permanent.
- Decreased range of motion, mobility is impaired. Dystrophic changes in the articular cartilage lead to the loss of normal motor activity. It is difficult for a person to make simple movements: tilts, turns.
- The development of the pathological process in the form nerve root damage. For this reason, the patient may notice changes in the sensitivity in the legs, while it can both decrease and increase.
- In more severe cases, there is dysfunction of the pelvic organs: problems with urination, erectile dysfunction.
The true reason that causes such changes in the spine has not yet been established. Only a number of factors predisposing to this disease are known:
- Sedentary lifestyle. Osteochondrosis is often called "office disease", because such workers spend most of their time sitting at the table. As a result, muscle tissue loses its tone and lends itself to excessive relaxation.
- Disruptions in the hormonal background. Hormonal disorders from the endocrine system and sexual can negatively affect nutrition cartilage tissue spine, which increases the risk of dystrophic pathologies.
- Congenital diseases of the musculoskeletal system. Patients who already have similar problems, for example: curvature of the limbs or flat feet, are most susceptible to osteochondrosis.
- Regular physical activity, incommensurable with the physiological capabilities of the spine. Although sport is a good prevention of the disease, but excessive passion for it can lead to the opposite - provoke its development.
How is the disease treated today
Unfortunately, it is impossible to completely get rid of the disease, however, starting treatment at stages 1-2, it is quite possible to achieve high therapeutic results and achieve stable remission. Pathology therapy methods imply an integrated approach, the task of which is as follows:
- reduction of pain in the lumbar region and sacrum;
- elimination of muscle tension, elimination of spasms;
- increased tone of the muscles of the back, buttocks, lower extremities;
- stopping the inflammatory process, improving the nutrition of cartilage tissue;
- increasing the patient's motor activity, eliminating disorders in the functioning of the pelvic organs (if any).
What medications can be prescribed? The doctor individually paints a treatment regimen and selects the most optimal options for medicines.
In addition, you should be aware of such a concept as first aid for exacerbation. It consists in giving a person peace, it is necessary to adhere to bed rest, and tie a warm scarf on the lumbar region, that is, provide dry heat.
The drug Analgin.
An integral part of therapy is the use of non-steroidal anti-inflammatory drugs - NSAIDs. Their task is to eliminate the inflammatory process, swelling, and reduce pain. In the case when there is a pronounced spasm, the doctor prescribes muscle relaxants - drugs that relax the muscles.
You will also need the use of chondroprotectors, they improve the nutrition of cartilage, inhibit the progression of pathology.
Together with NSAIDs and chondroprotectors, local treatment is prescribed in the form of ointments / gels of the same pharmacological groups.

A referral to physiotherapy is mandatory. Such methods well relieve pain, improve the general well-being of the patient and increase the effectiveness of local drugs. The most commonly recommended procedures are:
- Phonophoresis(exposure to ultrasonic waves).
- Darsonvalization(use of alternating pulsed current).
- Magnetic resonance treatment(the method is based on nuclear spin magnetic resonance). It should not be confused with MRI diagnostics, although the study operates on the same technology.
Another type of therapy that cannot be ruled out in any way is physiotherapy(LFK). Thanks to correctly selected exercises, the patient can strengthen muscle tissue and at the same time have a relaxing effect. Exercise therapy is used not only in combination with the main methods, but also comes first during the rehabilitation period after surgery.

A set of exercises for the lower back.
The appointment of the operation is provided in extreme cases, when all possible methods of therapy were previously tried, but they did not give the desired result. Also, surgery is prescribed in the later stages of the pathology, which no longer provides for a conservative impact.
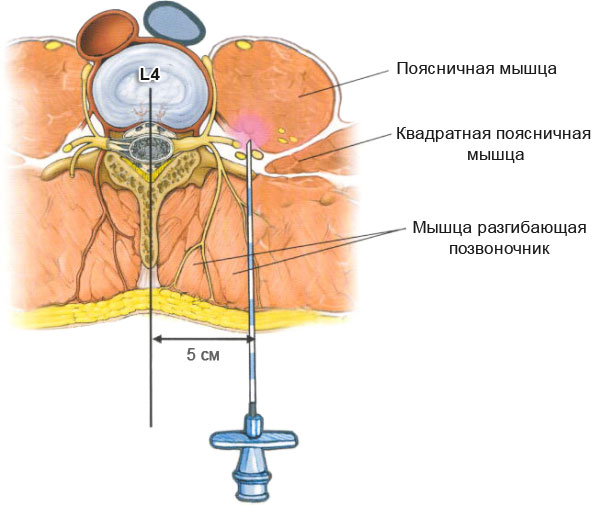
Use of injections
In some cases, injection of drugs is simply necessary. As a rule, injections are prescribed during an exacerbation, when there is a sharp pain during a pinched nerve endings.
By introducing medications in the form of injections, the active substances almost instantly reach the focus of inflammation and stop the pain syndrome. In addition, they bypass the digestive organs, thereby not injuring their mucosa.
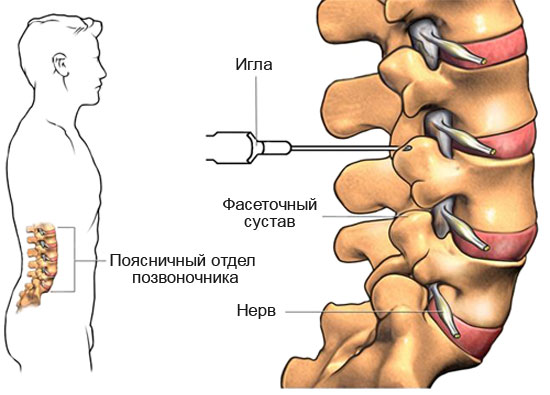
Penetration of the needle to the spine.
You can use a variety of types of injection of the drug:
| Type of injection | For what purpose is it used |
| Injection in the gluteal muscle (intramuscular) | In most cases, they use it. The active substance rapidly penetrates into the bloodstream and has the necessary therapeutic effect. |
| intravenous | Apply if necessary, immediate action, in order to eliminate the inflammatory process and stop spasm. |
| Subcutaneous | During the treatment of osteochondrosis, he recommends subcutaneous injection of B vitamins, so they can get the highest possible result. |
| Therapeutic blockade | The drug is injected directly into the focus of inflammation. More often, novocaine blockades are used, with the aim of quickly, effectively and for as long as possible to eliminate pain. |
Why do patients often resort to injections, what are their advantages?
- Rapid therapeutic effect, high efficiency. Due to the fact that the drug bypasses the digestive tract and enters the circulatory system quickly, it retains its effectiveness as much as possible, in contrast to the oral use of drugs.
- Preservation of the exact dosage of the active substance. When injected, the exact dosage of the drug is maintained, and when taken orally, part of the active ingredients is lost due to the effect of enzymes (digestive enzymes) on them.
- Reduced risk of side effects. Means used for the treatment of osteochondrosis and other pathologies of the musculoskeletal system contain components that negatively affect the mucous membrane of the digestive tract. When injected, the contents bypass this system, thereby reducing the formation of inflammatory processes.
Often, injections for osteochondrosis become the only salvation, because because of pain, a person often cannot even move. However, it should be understood that the injection should only be trusted by a specialist who understands how much the drug needs to be injected, and most importantly, which one.
If necessary, relieve pain and eliminate muscle spasms, a course of painkillers and antispasmodics is prescribed, usually the duration of use is 5-10 days, sometimes depending on the severity of the symptoms.
Drugs for exacerbation, injection anesthesia:

The drug Baralgin.
In addition to the above remedies, it is recommended to use a number of vitamin remedies, in this case, these are B vitamins. They have a beneficial effect on the state of nerve endings, improve blood circulation, and reduce the duration of the pain period.
At the same time, local influence can be used. For example, Diclofenac ointment will help well with the manifestation of pain, reduce the overall severity of symptoms. Darsonval and Dimexide will also give good results, so it is advisable to use them in conjunction with injections.
In addition to standard injections, there are medical blockades in the treatment of osteochondrosis. It is immediately worth noting that they are not a means of treatment, but only allow you to quickly eliminate the symptoms of pathology. For blockades, painkillers are used, which are injected directly into the focus.
Recently, homeopathic injections have gained popularity. The drugs used are made on the basis of natural raw materials, and according to some experts, they do a pretty good job of relieving pain. There are the following, the most effective medicines for signs of osteochondrosis:
- Target T;
- coenzyme;
- Traumeel S.
During the period when the disease worsens, oral painkillers practically do not work, it is unbearable to endure pain, so injections come to the rescue. However, it is highly not recommended to prescribe them on your own, here you need to trust an experienced neurologist.
exercise therapy
In addition to drug therapy and massage, there is another method of treatment that gives good results and is guaranteed to help in improving the overall health of the patient - exercise therapy. Therapeutic gymnastics is aimed at strengthening the muscular corset of the back, ligaments of the buttocks and the femoral region, which is extremely necessary for dystrophic processes of the musculoskeletal system.
A set of exercises is selected exclusively by the attending physician, the main thing here is not to harm the patient and take into account all the necessary parameters: age, stage of pathology, general physical condition. Therefore, exercise therapy is selected exclusively on an individual basis, after a thorough history taking.
It is important for the patient to adhere only to the complex that the specialist appointed and selected, while not making his own adjustments.
Please note that when performing exercises, you should not experience pain, minor pain is allowed, which does not cause obvious discomfort.
Important! Physical education is not carried out during the period of exacerbation of osteochondrosis, only after stopping its pronounced clinical picture. The same applies to acupuncture, the use of medicinal leeches, baths / saunas.
- practice daily, do not be lazy;
- perform all exercises slowly, carefully, without sudden movements;
- breathe properly - deep breath, slow exhalation;
- consult with your doctor, report all points.
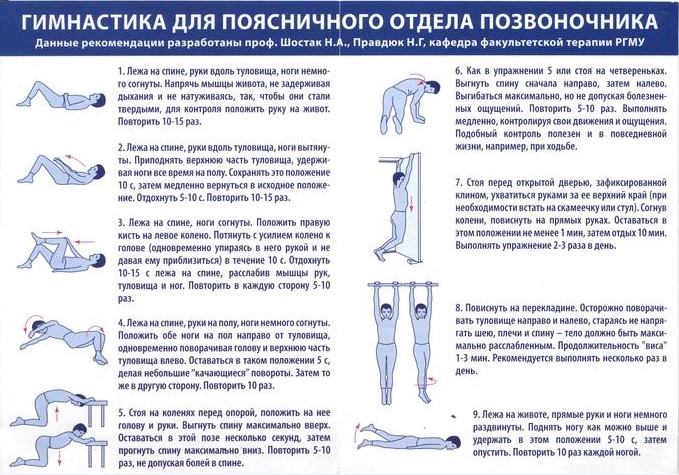
A set of exercises.
Please note again that the course is selected individually, from the general base of exercise therapy, you can use the following:
- Starting position lying on your back. You should lie down on a hard, flat surface, you can use the floor and a yoga mat. Bend your knees, arms straight, palms on the floor. Slowly raise the pelvis, tear it off the floor by 10-20 cm, hold it for a couple of seconds, lower it as you exhale. The recommended number of times is 10-15.
- Roll over on your stomach, stretch your arms forward, palms down. On inspiration, raise one arm and slightly bend in the back, on exhalation, return to the starting position. Then we repeat the same with the other hand. Perform if possible 10-15 times.
- Starting position lying on your back. The arms are straight, along the body, the legs are also straightened. Slowly bend your knees and try to reach them to the stomach, while exhaling, straighten back.
Such procedures should be repeated daily, and preferably several times, to achieve maximum effect. Yoga, swimming, stretching won't hurt either.
What pain can be
It is impossible to avoid the development of pain syndrome in lumbar osteochondrosis, since there are many nerve endings in this section. The classic manifestation is radicular syndrome, which is characterized by compression of the spinal nerves. Against this background, the patient complains of a number of symptoms, exacerbation and severe pain in the first place.
In neurology, with this diagnosis, it is customary to divide the pain syndrome in osteochondrosis into three forms:
- chronic;
- subacute;
- acute.
Pain syndrome of acute type with simultaneous lumbago in medical terminology is called lumbago. It can last several minutes, sometimes about an hour, while it proceeds paroxysmal. The pain itself has a stabbing character, localized deep in the tissues. However, there may be a burning sensation and numbness in the area of the pathological focus. The total duration of lumbago is up to 7 days, but, as a rule, the syndrome stops in the next few days.
The chronic form and subacute, most often occurs against the background of hypothermia or after physical exertion. It should be noted that the pain in this case has a slow development and is mainly noted on the left or right side of the lower back, aggravated by bending, turning. The chronic form is not difficult to distinguish, it can disturb a person for 2-4 weeks or more, and also give it to the legs or thigh.
States 1, 2, 3, 4, degrees
Diseases of the musculoskeletal system, like any other pathology, have their own stages. In the practice of traumatology, it is customary to distinguish four degrees of degenerative disorders of the intervertebral discs of the lumbar spine.
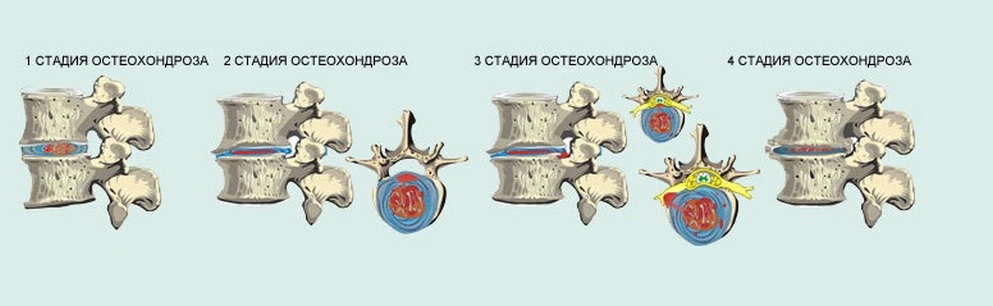
At 1st degree pathological changes are still insignificant, the clinical picture is mild, symptoms are rare. Also occasionally there are pains and mainly with active movements (this can be turning the body, active physical activity, or simply lifting heavy objects).
Although the first degree is characterized by minimal changes, they already exist and, if detected, treatment should not be postponed.
diagnosing 2 degrees occurs on the basis of the patient's complaints about the development of pain in the lower back and its irradiation to the gluteal region. At this stage, the signs of the disease become more pronounced, become permanent, and painful sensations are possible even without exertion or sudden movements. The second stage is characterized by a change in the shape of the disc, it becomes flatter, the nerve endings are compressed. This phenomenon is called protrusion, which in the future can provoke the formation of a vertebral hernia.
If at stage 1 it is still possible to influence therapeutic massages and exercise therapy, then for the second this will not be enough, drug therapy is already connected.
At 3 degrees dystrophic changes, a rupture of the fibrous ring is diagnosed, followed by leakage of the constituent secret. All this is accompanied by constant, aching pain, movements are significantly limited, and problems with internal organs are possible.
In case of occurrence 4 degrees all dystrophic processes in the spine are irreversible. The following happens: the growth of cartilage tissue, which leads to a severe limitation in mobility, and then to disability. In addition, there is compression of the nerves of the spinal canal and this is what causes paralysis.
Osteochondrosis of the lumbar is a serious ailment that requires immediate treatment under the supervision of an experienced specialist. All stages of therapy should be aimed at improving blood flow and tissue nutrition, reducing the inflammatory process, pain, and spasms. The result should be - the achievement of stable remission.
Exacerbation during pregnancy
Pregnancy is the most "tender" period in the life of every woman, since any negative changes in the body can harm not only the expectant mother, but also the child.
Osteochondrosis is no exception, although it is not capable of provoking congenital pathologies, it can become one of the factors that can terminate a pregnancy, especially in its early stages.
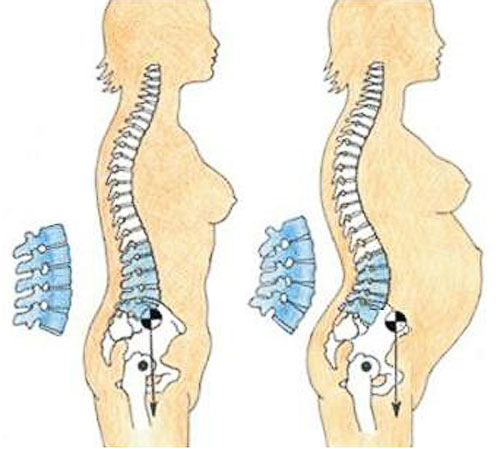
What does osteochondrosis look like during pregnancy.
If we consider a disease that occurs immediately at the time of bearing a child, then its main causes are the rapid weight gain of a woman, which creates a load on the spine, a decrease in motor activity and a restructuring of the hormonal background.
The problematic of therapy lies in contraindications to taking medications, as they can adversely affect the child himself. It remains only to use the well-known Diclofenac in the form of ointments or in tablet form, but in a very small dose and with a minimum course. It is also possible to use some exercise therapy procedures, but only under the supervision of an appropriate specialist - a rehabilitation therapist, a neurologist.
Is it possible to bathe in the bath
This question is often asked to neurologists, especially by those patients who like to spend time in a sauna or bath. Reasoning about this is very ambiguous, because on the one hand, the steam room is beneficial for the body, it is a kind of detox, and on the other hand, it can be harmful. To bathe or not to bathe should be decided solely by the attending physician, because it will depend on many factors: the stage of the disease, how it manifests itself, the presence of concomitant diseases, and so on.
It is also a fact that osteochondrosis is accompanied by structural changes in cartilaginous joints, due to which pain syndrome develops. When visiting the steam room, the fluid output increases, due to which the pain can increase many times over.
Of course, in addition to such a negative factor, there are also positive aspects, for example: heat improves blood circulation, cleanses the lungs, and helps to remove toxins through the skin.
Is it possible to cure the spine with the help of a bath? Unfortunately not and this is the reality.. Sauna, bath, of course, they can have a positive effect on the entire body, but by no means are they a panacea for all diseases. Therefore, beforehand, it is necessary to visit a doctor, consult with him and get the right answer, is it possible to bathe or is it better to abstain.
For the treatment and prevention of DISEASES OF THE JOINTS and SPINE, our readers use the method of fast and non-surgical treatment recommended by the leading rheumatologists of Russia, who decided to oppose pharmaceutical lawlessness and presented a medicine that REALLY TREATS! We got acquainted with this technique and decided to bring it to your attention.
It is important to note that this disease cannot be neglected. As usual, when such a diagnosis was made: "It's okay, how dangerous it can be, you can drink painkillers and it will pass." In fact, nothing just goes away and back pain requires immediate treatment. It should be understood that such a pathology is accompanied by extremely dangerous complications.
It is easy to influence the disease in the initial stages, as soon as the first symptoms appear, and very difficult when it has "taken deep roots" (you can maintain a more or less normal state of the spine, but in the later stages, returning to a normal, former lifestyle is no longer possible ).
And remember, the best treatment is the timely prevention of a healthy spine and the body as a whole.
No need to treat joints with pills!
Have you ever experienced unbearable joint pain? Judging by the fact that you are reading this article, you or your loved ones are faced with this problem. And you know firsthand what it is:
- inability to move easily and comfortably;
- discomfort when going up and down stairs;
- unpleasant crunch, clicking not of their own free will;
- pain during or after exercise;
- inflammation in the joints and swelling;
- causeless and sometimes unbearable aching pain in the joints ...
Surely you have tried a bunch of medicines, creams, ointments, injections, doctors, examinations, and, apparently, none of the above has helped you ... And there is an explanation for this: it is simply not profitable for pharmacists to sell a working drug, as they will lose clients! It was precisely against this that the leading rheumatologists and orthopedists of Russia jointly opposed, presenting the long-known among the people effective remedy from PAIN IN THE JOINTS, which REALLY CURES, and not just relieves pain!
Check out the reviews of patients who have undergone treatment abroad. In order to receive information about the possibility of treatment for your case, leave us a request for treatment at this link.
Be sure to consult your doctor before treating diseases. This will help to take into account individual tolerance, confirm the diagnosis, make sure the treatment is correct and exclude negative drug interactions. If you use prescriptions without consulting a doctor, then this is entirely at your own risk. All information on the site is presented for informational purposes and is not a medical aid. You are solely responsible for the application.
All diseases are distributed by international classification. So, spinal osteochondrosis code for ICD 10 has 42. The International Classification of Diseases was invented to facilitate the processing of medical information. Moreover, in connection with the law on non-disclosure of the diagnosis, it is the disease code that is written on the patient's card, and not its name. This helps to protect a person from the spread of the diagnosis, since only a medical worker knows the code of the tenth international classification. Disease coding usually includes letters and numbers.
For information
Revision of international classification codes is ongoing. Each version is somewhat different from the previous one. Now all doctors use the ICD 10 code to designate the disease.
The tenth issue is characterized by the following classification of osteochondrosis of the spine:
- 1 Osteochondrosis of the spine in the classical sense and clinical manifestation is coded M42. All other varieties begin with the same number, but then comes the subspecies number, which indicates the features of the manifestation of the disease.
- 2 For a disease that is localized in the region of the cervical vertebrae, the number M42.02 is characteristic. At the same time, for the cervicothoracic region, the classification assigned the code M42.03.
- 3 In ICD 10, osteochondrosis belongs to class 13. Letter coding allows you to encrypt a lot of information for specialists to make it easier to prescribe treatment. Each letter is assigned to a particular class.
All clinical manifestations of the disease are classified by experts as a subclass of dorsopathy. It has the code M40-M54. Hence, it turns out that osteochondrosis of the spine is classified as M42. It is in this interval of alphanumeric values that all diseases that are associated with the human body fit.
Usually, in patients who have such a code in the "diagnosis" line in their outpatient card, there is a pathology associated with the spine and the connective tissues and muscles adjacent to it. Usually a person complains of constant severe pain in the back. The symptoms are explained as follows:
- the presence of spinal injuries, inflammatory processes, developmental pathology;
- stretching of the ligaments of the spinal column.
In the presence of such complaints, the specialist can safely diagnose a disease belonging to the class of dorsopathy.
Causes of osteochondrosis
Various deformities that are observed in the spine belong to the M40-M43 class. After this classification come the spondylopathies, which range from M45 to M49. But in the interval between codes M50 and M54, various subspecies of other changes in the spinal column are hidden.
A specialist can correctly classify the disease only after receiving the results of the examination. This takes into account the history of the disease, compression of the spinal cord. With the correct diagnosis, it is easy to prescribe adequate treatment.

Sometimes the diagnosis can be difficult due to comorbidities. So, kidney disease is manifested by pain in the lumbosacral region. If the specialist, after receiving the results, does not observe pathologies in this section of the spine, then he sends the patient for examination of the kidneys and intestines.
If problems with other parts of the spine are identified, it is necessary to additionally undergo an examination by a neurologist and a therapist.
To determine the condition of the intervertebral discs and identify the presence of a hernia and other neoplasms, an MRI is required. Such studies will show a completely complete picture of the mobility of the vertebrae. In the course of the study, the condition of the nearby muscles and connective tissues is checked, and the ligaments are examined.
Most often, the disease is diagnosed in the cervical, thoracic, lumbar regions.
Diseases cervical spine is a fairly common occurrence. Many patients complain of constant headaches that occur due to problems with the first vertebrae. Quite often there is a subluxation of the first vertebra. Usually this phenomenon occurs during a birth injury. When the first vertebra is dislocated, the entire spinal column is distorted, which often leads to such a phenomenon as scoliosis. Against this background, not only frequent headaches develop, but also dizziness, sleep problems, atherosclerosis and pressure problems.

In the region of the sternum, problems of the spine are observed quite rarely. This is due to anatomical features. It is this department that is practically immobile, therefore, it is not subjected to any serious negative impact and unnecessary injury.
Most often, pain is localized in the lumbar region, since the entire weight of a person falls on this particular section of the spine. The lower back also suffers from improper physical activity, when lifting all kinds of weights, a sedentary lifestyle.
Symptoms of the disease
Spinal problems in the lumbar region are the most common ailment. Quite often, people with complaints of back pain turn to specialists. Modern look life made the disease look younger, since 10 years ago problems were diagnosed no earlier than at 45 years old. Today, even teenagers suffer from this disease. This is due to the fact that a person has stopped moving, playing sports, walking.

Due to the constant sedentary lifestyle, the spine suffers, and primarily the lumbar. This is due to the fact that when sitting, the entire load falls precisely on the lower back. Cartilage and ligaments wear out and cause a lot of discomfort.
The main causes of back problems include:
- 1 sedentary lifestyle. This is especially true for people who work in an office or have to spend a lot of time driving a car.
- 2 Heavy lifting and exorbitant exercise stress. Most often, loaders, athletes and bodybuilders tear off their backs. Permanent injuries of the spine are superimposed on each other, which leads to serious diseases.
- 3 Changes in the hormonal background in the elderly. They can provoke changes in the bone apparatus. The spine is no longer supported by elastic and strong muscles, the vertebrae descend and begin to rub against each other.
- 4 Heredity. Usually, osteochondrosis is transmitted through the generation, so very often the youngest children in the family suffer from such an ailment literally from birth.
- 5 Injuries of the spinal column. As a result, their osteochondrosis develops quite quickly. We can say that it is a consequence of trauma.
The following main symptoms stand out:
- 1 Severe pain in the back. If pinching occurs, then pain may be in other organs.
- 2 Problems with the muscles of the legs, pain in the lower extremities, cramps, poor circulation.
- 3 Loss of sensation in the entire lower part of the body.
- 4 Disorders of the reproductive system of the body are observed, sensitivity is lost as a result of poor blood circulation.
- 5 When the course of the disease is neglected, problems with bowel movements of the bladder and intestines are observed.
- 6 Loss of pulse as a result of severe pain shock due to spasms of the arteries.
- 7 Dry skin.
- 8 Interruptions in the work of the systems of internal organs located in the abdominal cavity.
At the moment, experts continue to explore and supplement the ICD-10.
Some believe that the symptoms of osteochondrosis can be attributed to the interval of diseases M50-M54. They believe that it will be correct to define the disease to other dorsopathies, and not to classify it as deforming dorsopathies.
In medical practice, all diseases are classified according to ICD-10, osteochondrosis also has its own code. This encoding is mainly used for statistical data processing and protection of personal information. Osteochondrosis is characterized by degenerative changes in cartilage tissue, it is presented in the section of diseases of the musculoskeletal system - class XIII in the ICD 10th revision.
Diseases of the spine
 In ICD-10, in order to describe the destructive processes occurring in the intervertebral discs, they use the code M42. Usually the cipher consists of 4 characters, but to clarify the localization of the pathological process, 5 characters are indicated:
In ICD-10, in order to describe the destructive processes occurring in the intervertebral discs, they use the code M42. Usually the cipher consists of 4 characters, but to clarify the localization of the pathological process, 5 characters are indicated:
- The number 0 at the end of the code means that degenerative changes occur in several parts of the spine at once - common osteochondrosis.
- If at the end of the cipher the fifth number is 1, this indicates destruction in the first or second cervical vertebra.
- The number 2 corresponds to the localization of the pathology in the neck.
- The number 3 indicates that pathological changes occur in the segments of the cervicothoracic spine.
- To describe the pathology in the segments of the thoracic spine, the number 4 is used.
- The pathological process, localized in the lumbar-thoracic region, is described using the number 5.
- If the number 6 is indicated at the end of the code, then the destruction of the intervertebral discs occurs in the lumbar region.
- Osteochondrosis of the lumbosacral region is encrypted using the number 7.
- The number 8 speaks of the defeat of the sacral and coccyx.
- If during the examination of the patient the exact localization of the pathology is not established, use the number 9.
This classification is rarely used. Usually, a 4-digit code is enough to describe the disease.
What cipher is used in children?
The disease corresponds to the code M42.0. Degenerative changes in cartilage and bone tissue in children are classified as a separate group of diseases, since the clinical picture of the disease differs significantly from other types of osteochondrosis.
With the defeat of the cervical and thoracic region, pain is noted, but motor and sensory disorders in the shoulder girdle come to the fore. Pathology leads to curvature of the vertebrae, impaired posture. Chest deformity is also possible.
Often the disease is accompanied by symptoms such as shortness of breath and difficulty breathing, spontaneous fainting and poor tolerance for stress, both physical and mental.
What is the classification for adults?
 Code M42.1 is used to describe degenerative-dystrophic changes in the intervertebral discs in patients over 18 years of age. If the diagnosis is not confirmed by instrumental and laboratory studies, the ciphers from the heading M54 - dorsalgia are used for the description. If the patient's main complaint is not pain, use the code corresponding to the main symptom.
Code M42.1 is used to describe degenerative-dystrophic changes in the intervertebral discs in patients over 18 years of age. If the diagnosis is not confirmed by instrumental and laboratory studies, the ciphers from the heading M54 - dorsalgia are used for the description. If the patient's main complaint is not pain, use the code corresponding to the main symptom.
Interesting!
The diagnosis of osteochondrosis of the cervical spine in adults in the ICD-10 has the code M42.12.
Joint degeneration
In the advanced stages of the disease, degenerative changes can affect not only the intervertebral discs, but also the joints. In cases of juvenile osteochondrosis, ciphers are used to describe joint lesions:
- damage to the hip joints and pelvis - M91;
- other specified forms of juvenile pathology - M92.
To describe degenerative processes in the joints in adults, code from section M93 - other osteochondropathy is used. This category includes:
- Osteochondrosis of the carpal bone (lunate) coded as M93.1
- Osteochondritis dissecans affecting the joints is encrypted using the code M93.2
- For other specified osteochondropathy use code M93.8
- Unspecified osteochondropathy - M93.9.
At the first stages of treatment, if the diagnosis is not finally confirmed, codes from the category of arthrosis can be used. According to the established rules, the main diagnosis is indicated first, for example, cervical osteochondrosis, and then the concomitant ones.
Sensational discovery of doctors
After various studies, doctors have found a sensational way to successfully affect the joints.- A new remedy has appeared that completely cures joints!
- No painful procedures!
- Without the use of antibiotics!
- Result already in the FIRST WEEK!
Class XIII. OTHER DORSOPATHY (M50-M54)
Excludes: current injury - spinal injuries by area of the body discitis NOS ( M46.4)
M50 Injury of intervertebral discs of cervical region
Includes: cervical intervertebral disc lesions with pain syndrome
lesions of the intervertebral discs of the cervicothoracic region
M50.0+ Damage to the intervertebral disc of the cervical spine with myelopathy ( G99.2*)
M50.1 Damage to the intervertebral disc of the cervical spine with radiculopathy
Excludes: shoulder sciatica NOS ( M54.1)
M50.2 Displacement of the intervertebral disc of the cervical spine of another type
M50.3 Other cervical disc degeneration
M50.8 Other lesions of the intervertebral disc of the cervical region
M50.9 Cervical intervertebral disc lesion, unspecified
M51 Involvement of intervertebral discs of other departments
Includes: lesions of the intervertebral discs of the thoracic,
thoracic and lumbosacral regions
M51.0+ Lesions of the intervertebral discs of the lumbar and other parts with myelopathy ( G99.2*)
M51.1 Lesions of the intervertebral discs of the lumbar and other parts with radiculopathy
Sciatica due to damage to the intervertebral disc
Excludes: lumbar sciatica NOS ( M54.1)
M51.2 Another specified displacement of the intervertebral disc. Lumbago due to displacement of the intervertebral disc
M51.3 Other specified intervertebral disc degeneration
M51.4 Nodes [hernia] Schmorl
M51.8 Other specified lesion of intervertebral disc
M51.9 Disorder of intervertebral disc, unspecified
M53 Other dorsopathies, not elsewhere classified [see localization code above]
M53.0 Cervical-cranial syndrome. Posterior sympathetic syndrome
M53.1 Neck and shoulder syndrome
Excludes: cervical intervertebral disc disease ( M50. -)
infraraconic syndrome [brachial plexus lesion] ( G54.0)
M53.2 Spinal instability
M53.3 Sacrococcygeal disorders, not elsewhere classified. coccygodynia
M53.8 Other specified dorsopathies
M53.9 Dorsopathy, unspecified
M54 Dorsalgia [localization code see above]
Excludes: psychogenic dorsalgia ( F45.4)
M54.0 Panniculitis affecting the cervical region and spine
Excludes: panniculitis:
NOS ( M79.3)
lupus ( L93.2)
M35.6)
M54.1 radiculopathy
Neuritis and sciatica:
shoulder NOS
lumbar NOS
lumbosacral NOS
thoracic NOS
Sciatica NOS
Excludes: neuralgia and neuritis NOS ( M79.2)
radiculopathy with:
cervical intervertebral disc injury
department ( M50.1)
lumbar intervertebral disc injury
and other departments M51.1)
spondylosis ( M47.2)
M54.2 cervicalgia
Excludes: cervicalgia due to intervertebral disc disease ( M50. -)
M54.3 Sciatica
Excludes: sciatic nerve lesion ( G57.0)
sciatica:
caused by damage to the intervertebral disc M51.1)
with lumbago ( M54.4)
M54.4 Lumbago with sciatica
Excludes: due to damage to the intervertebral disc ( M51.1)
M54.5 Pain in the lower back. Lumbar pain. Tension in the lower back. Lumbago NOS
Excludes: lumbago:
due to displacement of the intervertebral disc M51.2)
with sciatica ( M54.4)
M54.6 Pain in the thoracic spine
Excludes: due to damage to the intervertebral disc ( M51. -)
M54.8 Other dorsalgia
M54.9 Dorsalgia, unspecified. Back pain NOS
SOFT TISSUE DISEASES ( M60-M79)
MUSCLE DISEASES (M60-M63)
Excludes: dermatopolymyositis ( M33. -)
muscular dystrophies and myopathies ( G71-G72)
myopathy with:
amyloidosis ( E85. -)
polyarteritis nodosa ( M30.0)
rheumatoid arthritis ( M05.3)
scleroderma ( M34. -)
Sjögren's syndrome ( M35.0)
systemic lupus erythematosus ( M32. -)
M60 Myositis [localization code see above]
M60.0 infectious myositis. Tropical pyomyositis
If necessary, to identify the infectious agent, use additional codes ( B95-B97).
M60.1 Interstitial myositis
M60.2 Soft tissue granuloma due to foreign body, not elsewhere classified
Excludes: granuloma of skin and subcutaneous tissue due to foreign body ( L92.3)
M60.8 Other myositis
M60.9 Myositis, unspecified
M61 Muscle calcification and ossification [localization code above]
M61.0 Myositis ossificans traumatic
M61.1 Myositis ossificans progressive. Fibrodysplasia ossificans, progressive
M61.2 Paralytic calcification and ossification of muscles. Myositis ossificans with quadriplegia or paraplegia
M61.3 Muscle calcification and ossification associated with burns. Myositis ossificans associated with burns
M61.4 Other muscle calcification
Excludes: calcific tendonitis ( M65.2)
shoulder ( M75.3)
M61.5 Other muscle ossification
M61.9 Muscle calcification and ossification, unspecified
M62 Other disorders of muscle [localization code above]
Excludes: convulsions and spasm ( R25.2)
myalgia ( M79.1)
myopathy:
alcoholic ( G72.1)
medicinal ( G72.0)
"stiff person" syndrome G25.8)
M62.0 Divergence of the muscle
M62.1 Other muscle tear (non-traumatic)
Excludes: tendon rupture ( M66. -)
traumatic muscle rupture - muscle injuries in areas of the body
M62.2 Ischemic muscle infarction
Excludes: compression syndrome ( T79.6)
traumatic muscle ischemia ( T79.6)
Volkmann's ischemic contracture ( T79.6)
M62.3 Immobilization syndrome (paraplegic)
M62.4 Muscle contracture
Excludes: joint contracture ( M24.5)
M62.5 Muscle wasting and wasting, not elsewhere classified
Muscle atrophy in the absence of a functional load on them NEC
M62.6 Muscular deformity
Excludes: current injury - muscle injury over body area
M62.8 Other specified muscle lesions. Muscular hernia (shells)
M62.9 Muscle disorders, unspecified
M63* Muscle disorders in diseases classified elsewhere
Excludes: myopathy with:
endocrine diseases ( G73.5*)
metabolic disorders ( G73.6*)
Excludes: chronic crepitant synovitis of hand and wrist ( M70.0)
current injury - see ligament or tendon injuries by area of the body
soft tissue diseases associated with stress, overload and pressure ( M70. -)
M65.0 Tendon sheath abscess
If it is necessary to identify the bacterial agent, use an additional code ( B95-B96).
M65.1 Other infectious (teno) synovitis
M65.2 Calcific tendinitis
Excluded: shoulder ( M75.3)
specified tendonitis ( M75-M77)
M65.3 Snapping finger. Nodular disease of the tendon
M65.4 Tenosynovitis of the styloid process of the radius [de Quervain's syndrome]
M65.8 Other synovitis and tenosynovitis
M65.9 Synovitis and tenosynovitis, unspecified
M66 Spontaneous rupture of synovial membrane and tendon [localization code see above]
Includes: tissue tears caused by the application of conventional
efforts, as a result of a decrease in the strength of tissues
Excludes: rotator impingement syndrome ( M75.1)
traumatic rupture (when excessive force is applied to normal tissues) - tendon injuries along
areas of the body
M66.0 Rupture of the popliteal cyst
M66.1 Synovial rupture. Synovial cyst rupture
Excludes: popliteal cyst rupture ( M66.0)
M66.2 Spontaneous rupture of the extensor tendons
M66.3 Spontaneous flexor tendon rupture
M66.4 Spontaneous rupture of other tendons
M66.5 Spontaneous rupture of unspecified tendons. Rupture of the musculotendinous junction, non-traumatic
M67 Other disorders of synovial membranes and tendons
Excludes: Dupuytren's palmar fascial fibromatosis ( M72.0)
tendinitis NOS ( M77.9)
xanthomatosis localized in the tendons ( E78.2)
M67.0 Short calcaneal [Achilles] tendon (acquired)
M67.1 Other contracture of the tendon (sheath)
Excludes: with joint contracture ( M24.5)
M67.2 Synovial hypertrophy, not elsewhere classified
Excludes: villous-nodular [villonodular] synovitis, (pigmented) ( M12.2)
M67.3 migratory synovitis. Toxic synovitis
M12.3)
M67.4 Ganglion. Ganglion of a joint or tendon (sheath)
Excludes: cyst:
synovial bag)
synovial membrane) ( M71.2-M71.3)
ganglion in yaws ( A66.6)
M67.8 Other specified lesions of synovium and tendon
M67.9 Synovial and tendon lesion, unspecified
M68* Disorders of synovial membranes and tendons in diseases
classified elsewhere
M68.0* Synovitis and tenosynovitis in bacterial diseases classified elsewhere
Synovitis and tenosynovitis with:
gonorrhea ( A54.4+)
syphilis ( A52.7+)
tuberculosis ( A18.0+)
M68.8* Other disorders of the synovium and tendons in diseases classified elsewhere
OTHER SOFT TISSUE DISEASES (M70-M79)
M70 Soft tissue disorders associated with exercise, overload and pressure [localization code above]
Includes: occupational soft tissue diseases
Excludes: bursitis:
NOS ( M71.9)
shoulder ( M75.5)
enthesopathy ( M76-M77)
M70.0 Chronic crepitant synovitis of the hand and wrist
M70.1 Bursitis of the hand
M70.2 Bursitis of the olecranon
M70.3 Other bursitis of the elbow
M70.4 Prepatellar bursitis
M70.5 Other bursitis of the knee
M70.6 Bursitis of the greater trochanter (femur). Tendonitis of the greater trochanter
M70.7 Other hip bursitis. ischial bursitis
M70.8 Other soft tissue diseases associated with stress, overload and pressure
M70.9 Unspecified soft tissue disorders associated with stress, overload and pressure
M71 Other bursopathies [see localization code above]
Excludes: bunion of the big toe ( M20.1)
bursitis associated with exercise, congestion, and pressure ( M70. -)
enthesopathy ( M76-M77)
M71.0 Bursal abscess
M71.1 Other infectious bursitis
M71.2 Synovial cyst of the popliteal region [Baker]
Excluded: with a gap ( M66.0)
M71.3 Another bursal cyst. Synovial cyst NOS
Excludes: synovial cyst with rupture ( M66.1)
M71.4 Calcium deposition in the synovial sac
Excluded: in the shoulder ( M75.3)
M71.5 Other bursitis, not elsewhere classified
Excludes: bursitis:
NOS ( M71.9)
shoulder ( M75.5)
collateral tibial
Pellegrini-Stidy ( M76.4)
M71.8 Other specified bursopathies
M71.9 Bursopathy, unspecified. Bursitis NOS
M72 Fibroblastic disorders [localization code above]
Excludes: retroperitoneal fibromatosis ( D48.3)
M72.0 Palmar fascial fibromatosis [Dupuytren]
M72.1 Connective tissue nodules on the dorsum of the fingers
M72.2 Plantar fascial fibromatosis. plantar fasciitis
M72.3 nodular fasciitis
M72.4 Pseudosarcomatous fibromatosis
M72.5 Fasciitis, not elsewhere classified
Excludes: fasciitis:
diffuse (eosinophilic) ( M35.4)
nodular ( M72.3)
plantar ( M72.2)
M72.8 Other fibroblast disorders
M72.9 Fibroblast disorders, unspecified
M73* Soft tissue disorders in diseases classified elsewhere [see localization code above]
M73.0* Gonococcal bursitis ( A54.4+)
M73.1* Syphilitic bursitis ( A52.7+)
M73.8* Other soft tissue disorders in diseases classified elsewhere
M75 Shoulder disorders
Excludes: shoulder-hand syndrome ( M89.0)
M75.0 Adhesive capsulitis of the shoulder. "Frozen Shoulder" Shoulder periarthritis
M75.1 Shoulder rotator compression syndrome. Rotator compression or suprastenal incision or tear (complete) (incomplete), not specified as traumatic. Supraspinal syndrome
M75.2 biceps tendinitis
M75.3 Calcific tendonitis of the shoulder. Calcium deposition in the synovial sac of the shoulder
M75.4 Shoulder Impact Syndrome
M75.5 shoulder bursitis
M75.8 Other shoulder lesions
M75.9 Shoulder injury, unspecified
M76 Enthesopathies of lower limb, excluding foot [localization code see above]
Note The descriptive terms "bursitis", "capsulitis" and "ten dinitis" are often used without clear differentiation.
for various disorders of peripheral ligaments or muscle attachments; most of these conditions are grouped together under the term 'enthesopathy', which is common to lesions at these sites.
Excludes: bursitis due to exercise, overload and pressure ( M70. -)
M76.0 Gluteal tendonitis
M76.1 Tendinitis of the lumbar muscles
M76.2 Spur of the iliac crest
M76.3 iliac tibial ligament syndrome
M76.4 Tibial collateral bursitis [Pellegrini-Stidy]
M76.5 Patellar tendonitis
M76.6 Tendinitis of the calcaneal [Achilles] tendon. Calcaneal [Achilles] tendon bursitis
M76.7 Tendinitis of the fibula
M76.8 Other enthesopathies of the lower extremity, excluding the foot. Tibialis anterior syndrome
Tibialis posterior tendonitis
M76.9 Enthesopathy of lower limb, unspecified
M77 Other enthesopathies [localization code see above]
Excludes: bursitis:
NOS ( M71.9)
due to load, overload and pressure ( M70. -)
osteophyte ( M25.7)
enthesopathy of the spine M46.0)
M77.0 Medial epicondylitis
M77.1 Lateral epicondylitis. tennis elbow
M77.2 Periarteritis of the wrist
M77.3 Heel spur
M77.4 Metatarsalgia
Excludes: Morton's metatarsalgia ( G57.6)
M77.5 Other foot enthesopathy
M77.8 Other enthesopathies not elsewhere classified
M77.9 Enthesopathy, unspecified. Bone spur NOS. Capsulitis NOS. Periarthritis NOS. Tendinitis NOS
M79 Other soft tissue diseases, not elsewhere classified [localization code above]
Excludes: soft tissue pain, psychogenic F45.4)
M79.0 Rheumatism, unspecified. Fibromyalgia. Fibrositis
Excludes: palindromic rheumatism ( M12.3)
M79.1 Myalgia
Excluded: myositis ( M60. -)
M79.2 Neuralgia and neuritis, unspecified
Excludes: mononeuropathies ( G56-G58)
radiculitis:
NOS )
shoulder) ( M54.1)
lumbosacral)
sciatica ( M54.3-M54.4)
M79.3 Panniculitis, unspecified
Excludes: panniculitis:
lupus ( L93.2)
neck and spine M54.0)
recurrent [Weber-Christian] ( M35.6)
M79.4 Hypertrophy of the (popliteal) fat pad
M79.5 Residual foreign body in soft tissue
Excludes: granuloma (caused by foreign body in):
skin and subcutaneous tissue L92.3)
soft tissue ( M60.2)
M79.6 Pain in the limb
M79.8 Other specified soft tissue lesions
M79.9 Soft tissue disease, unspecified
OSTEOPATHY AND CHONDROPATHY
(M80-M94)
BONE DENSITY AND STRUCTURE DISORDERS
(M80-M85)
M80 Osteoporosis with pathological fracture [local code see above]
Inclusions: osteoporotic destruction and wedging of a vertebra
M48.5)
pathological fracture NOS ( M84.4)
wedge-shaped deformity of a vertebra NOS ( M48.5)
M80.0 Postmenopausal osteoporosis with pathologic fracture
M80.1 Osteoporosis with pathological fracture after ovariectomy
M80.2 Osteoporosis with pathological fracture caused by immobility
M80.3 Post-surgical osteoporosis with pathologic fracture due to intestinal malabsorption
M80.4 Drug-induced osteoporosis with pathological fracture
M80.5 Idiopathic osteoporosis with pathologic fracture
M80.8 Other osteoporosis with pathologic fracture
M80.9 Osteoporosis with pathological fracture, unspecified
M81 Osteoporosis without pathological fracture [localization code see above]
Excludes: osteoporosis with pathologic fracture ( M80. -)
M81.0 Postmenopausal osteoporosis
M81.1 Osteoporosis after ovary removal
M81.2 Osteoporosis due to immobility
Excludes: Sudeck's atrophy ( M89.0)
M81.3 Post-surgical osteoporosis due to malabsorption
M81.4 Drug osteoporosis
An additional external cause code (class XX) is used to identify the medicinal product.
M81.5 Idiopathic osteoporosis
M81.6 Localized osteoporosis [Lequena]
Excludes: Sudeck's atrophy ( M89.0)
M81.8 other osteoporosis. Senile osteoporosis
M81.9 Osteoporosis, unspecified
M82* Osteoporosis in diseases classified elsewhere [localization code above]
M82.0* Osteoporosis in multiple myelomatosis ( C90.0+)
M82.1* Osteoporosis in endocrine disorders ( E00-E34+)
M82.8* Osteoporosis in other diseases classified elsewhere
M83 Adult osteomalacia [see localization code above]
Excludes: osteomalacia:
children's and youth ( E55.0)
vitamin D-resistant ( E83.3)
renal osteodystrophy ( N25.0)
rickets (active) ( E55.0)
consequences ( E64.3)
vitamin D-resistant ( E83.3)
M83.0 Postpartum osteomalacia
M83.1 Senile osteomalacia
M83.2 Osteomalacia due to malabsorption. Post-surgical osteomalacia in adults due to malabsorption
M83.3 Osteomalacia in adults due to malnutrition
M83.4 Bone disease associated with aluminum
M83.5 Other medicinal osteomalacia in adults
If necessary, to identify the medicinal product, use an additional external cause code (class XX).
M83.8 Other osteomalacia in adults
M83.9 Osteomalacia in adults, unspecified
M84 Disorders of bone integrity [localization code above]
M84.0 Poor fracture healing
M84.1 Fracture nonunion [pseudarthrosis]
Excludes: pseudarthrosis after fusion or arthrodesis ( M96.0)
M84.2 Delayed fracture healing
M84.3 Stress fractures, not elsewhere classified. Stress fractures NOS
Excludes: overload [stress] fracture of the spine ( M48.4)
M84.4 Pathological fractures, not elsewhere classified. Pathological fracture NOS
Excludes: vertebral destruction NOS ( M48.5)
pathological fracture in osteoporosis ( M80. -)
M84.8 Other violations of the integrity of the bone
M84.9 Disruption of bone integrity, unspecified
M85 Other disorders of bone density and structure [localization code above]
Excludes: osteogenesis imperfecta Q78.0)
osteopetrosis [bone petrification] ( Q78.2)
osteopoikilosis ( Q78.8)
multiple fibrous dysplasia of bones ( Q78.1)
M85.0 Fibrous dysplasia (selective, one bone)
Excludes: fibrous dysplasia of jaw ( K10.8)
M85.1 Skeletal fluorosis
M85.2 Hyperostosis of the skull
M85.3 Osteitis due to the deposition of mineral salts (sclerosing)
M85.4 Single bone cyst
Excludes: solitary cyst of jaw bone ( K09.1-K09.2)
M85.5 Aneurysmal bone cyst
Excludes: aneurysmal cyst of the jaw bone ( K09.2)
M85.6 Other bone cysts
Excludes: jaw bone cyst NOS ( K09.1-K09.2)
generalized fibrocystic osteitis [Recklinghausen's bone disease] ( E21.0)
M85.8 Other specified disorders of bone density and structure. Hyperostosis of bones other than cranial
Excludes: diffuse idiopathic skeletal hyperostosis ( M48.1)
M85.9 Violation of bone density and structure, unspecified
OTHER OSTEOPATHIES (M86-M90)
Excludes: osteopathy after medical procedures ( M96. -)
M86 Osteomyelitis [localization code above]
If necessary, identify the infectious agent
use additional code ( B95-B97).
Excludes: osteomyelitis:
caused by salmonella A01-A02)
jaws ( K10.2)
spine ( M46.2)
M86.0 Acute hematogenous osteomyelitis
M86.1 Other forms of acute osteomyelitis
M86.2 Subacute osteomyelitis
M86.3 Chronic multifocal osteomyelitis
M86.4 Chronic osteomyelitis with drained sinus
M86.5 Other chronic hematogenous osteomyelitis
M86.6 Other chronic osteomyelitis
M86.8 Other osteomyelitis. Brodie's abscess
M86.9 Osteomyelitis, unspecified. Bone infection NOS. Periostitis without mention of osteomyelitis
M87 Osteonecrosis [localization code above]
Includes: avascular necrosis of bone
Excludes: osteochondropathy ( M91-M93)
M87.0 Idiopathic aseptic necrosis of bone
M87.1 Drug-induced osteonecrosis
If necessary, to identify the medicinal product, use an additional external cause code (class XX).
M87.2 Osteonecrosis due to trauma
M87.3 Other secondary osteonecrosis
M87.8 Other osteonecrosis
M87.9 Osteonecrosis, unspecified
M88 Paget's disease (of bones) [osteitis deformans] [localization code see above]
M88.0 Skull lesion in Paget's disease
M88.8 Damage to other bones in Paget's disease
M88.9 Paget's disease (of bones), unspecified
M89 Other diseases of bones [localization code see above]
M89.0 Algoneurodystrophy. Shoulder-hand syndrome. Zudek's atrophy. Sympathetic reflex dystrophy
M89.1 Premature fusion of the epiphysis with the diaphysis
M89.2 Other disorders of growth and development of bones
M89.3 Bone hypertrophy
M89.4 Other hypertrophic osteoarthropathy. Marie-Bamberger disease. Pachydermoperiostosis
M89.5 Osteolysis
M89.6 Osteopathy after polio
An additional code is used to identify past poliomyelitis ( B91).
M89.8 Other specified bone lesions. Cortical hyperostosis in children
Post-traumatic subperiosteal (periosteal) ossification
M89.9 Bone disease, unspecified
M90* Osteopathy in diseases classified elsewhere [see localization code above]
M90.0* Tuberculosis of the bones ( A18.0+)
Excludes: spinal tuberculosis ( M49.0*)
M90.1* Periostitis in other infectious diseases classified elsewhere
Secondary syphilitic periostitis ( A51.4+)
M90.2* Osteopathy in other infectious diseases classified elsewhere
Osteomyelitis:
echinococcal ( B67.2+)
gonococcal ( A54.4+)
salmonella ( A02.2+)
Syphilitic osteopathy or osteochondropathy ( A50.5+, A52.7+)
M90.3* Osteonecrosis in decompression sickness ( T70.3+)
M90.4* Osteonecrosis due to hemoglobinopathies ( D50-D64+)
M90.5* Osteonecrosis in other diseases classified elsewhere
M90.6* Deforming osteitis in neoplasms ( C00-D48+)
Osteitis deformans in malignant neoplasms in the bones ( C40-C41+)
M90.7* Fractures of bones in neoplasms ( C00-D48+)
Excludes: vertebral fracture due to neoplasms ( M49.5*)
M90.8* Osteopathy in other diseases classified elsewhere. Osteopathy in renal dystrophy ( N25.0+)
CHONDROPATHY (M91-M94)
Excludes: chondropathy after medical procedures ( M96. -)
M91 Juvenile osteochondrosis of hip and pelvis [localization code above]
Excludes: slippage of the upper epiphysis of the femur (non-traumatic) ( M93.0)
M91.0 Juvenile osteochondrosis of the pelvis
Juvenile osteochondrosis:
acetabulum
iliac crest [Buchanan]
ischiopubic synchondrosis [Van Neka]
pubic symphysis [Pearson]
M91.1 Juvenile osteochondrosis of the femoral head [Legg-Calve-Perthes]
M91.2
Coxa plan. Hip deformity after juvenile osteochondrosis
M91.3 Pseudocoxalgia
M91.8 Other juvenile osteochondrosis of the hip and pelvis. Juvenile osteochondrosis after elimination of congenital hip dislocation
M91.9 Juvenile osteochondrosis of the hip and pelvis, unspecified
M92 Other juvenile osteochondrosis
M92.0 Juvenile osteochondrosis of the humerus
Osteochondrosis (juvenile):
head of distal condyle of humerus [Panner]
head of humerus [Haas]
M92.1 Juvenile osteochondrosis of the radius and ulna
Osteochondrosis (juvenile):
lower ulna [burns]
head of radius [Brailsford]
M92.2 Juvenile osteochondrosis of the hand
Osteochondrosis (juvenile):
semilunar bone of the wrist [Kinbeck]
metacarpal heads [Mauclair]
M92.3 Other juvenile osteochondrosis of the upper extremities
M92.4 Juvenile osteochondrosis of the patella
Osteochondrosis (juvenile):
primary, patellar center [Kohler]
secondary, patellar center [Sinding-Larsen]
M92.5 Juvenile osteochondrosis of the tibia and fibula
Osteochondrosis (juvenile):
proximal end of the tibia [Blunt]
tibial tubercle [Osgood-Schlatter]
M92.6 Juvenile osteochondrosis of the tarsus
Osteochondrosis (juvenile):
Calcaneus [North]
abnormal bone located between the scaphoid
tarsal bone and head of the talus [Haglund]
talus [diaz]
navicular tarsal [Kohler]
M92.7 Juvenile osteochondrosis of the metatarsus
Osteochondrosis (juvenile):
fifth metatarsal [Izlena]
second metatarsal [Freiberga]
M92.8 Another specified juvenile osteochondrosis. Calcaneal apophysitis
M92.9 Juvenile osteochondrosis, unspecified
Apophysitis)
Epiphysitis) specified as juvenile,
Osteochondritis) of unspecified localization
Osteochondrosis)
M93 Other osteochondropathy
Excludes: spinal osteochondrosis ( M42. -)
M93.0 Slipping of the upper epiphysis of the femur (non-traumatic)
M93.1 Kienböck's disease in adults. Osteochondrosis of the semilunar bone of the wrist in adults
M93.2 Dissecting osteochondritis
M93.8 Other specified osteochondropathy
M93.9 Osteochondropathy, unspecified
Apophysitis)
epiphysitis) not specified as an adult or
Osteochondritis) juvenile, unspecified localization
Osteochondrosis)
M94 Other disorders of cartilage [see localization code above]
M94.0 Cartilaginous Rib Joint Syndrome [Tietze]
M94.1 Recurrent polychondritis
M94.2 Chondromalacia
Excludes: chondromalacia patella ( M22.4)
M94.3 Chondrolysis
M94.8 Other specified cartilage lesions
M94.9 Cartilage disorder, unspecified
OTHER musculoskeletal disorders
AND CONNECTIVE TISSUE (M95-M99)
M95 Other acquired deformities of the musculoskeletal system and connective tissue
Excluded: acquired(s):
absence of limbs and organs ( Z89-Z90)
limb deformities ( M20-M21)
congenital anomalies and deformities of the musculoskeletal system ( Q65-Q79)
deforming dorsopathies ( M40-M43)
maxillofacial anomalies [including malocclusion] ( K07. -)
musculoskeletal disorders after medical procedures ( M96. -)
M95.0 Acquired deformity of the nose
Excludes: deviated septum ( J34.2)
M95.1 Deformation of the auricle caused by trauma and subsequent perichondritis
Excludes: other acquired ear deformities ( H61.1)
M95.2 Other acquired head deformities
M95.3 Acquired neck deformity
M95.4 Acquired deformity of the chest and ribs
M95.5 Acquired deformity of the pelvis
Excluded: maternal care due to identified or suspected non-compliance
the size of the pelvis and fetus ( O33. -)
M95.8 Other specified acquired deformities of the musculoskeletal system
M95.9 Acquired deformities of the musculoskeletal system, unspecified
M96 Disorders of the musculoskeletal system following medical procedures, not elsewhere classified
Excludes: arthropathy accompanying intestinal shunt ( M02.0)
disorders associated with osteoporosis ( M80-M81)
the presence of functional implants and other prostheses ( Z95-Z97)
M96.0 Pseudarthrosis after fusion or arthrodesis
M96.1 Post-laminectomy syndrome, not elsewhere classified
M96.2 Post-radiation kyphosis
M96.3 Postlaminectomy kyphosis
M96.4 Post-surgical lordosis
M96.5 post-radiation scoliosis
M96.6 Fracture after placement of an orthopedic implant joint prosthesis or bone plate
Excludes: complications related to internal orthopedic devices, implants or
transplants ( T84. -)
M96.8 Other lesions of the musculoskeletal system after medical procedures
Joint instability due to removal of the joint prosthesis
M96.9 Disorders of the musculoskeletal system after medical procedures, unspecified
M99 Biomechanical disorders, not elsewhere classified
Note This rubric should not be used if the condition can be assigned to some other rubric.
The following additional fifth characters indicating the location of the lesion are given for optional use with the appropriate subcategories under the heading M99. -; see also the specified localization code on c644.
0 Head region cervico-occipital region
1 Neck region cervicothoracic region
2 Chest region lumbar-thoracic region
3 Lumbar region lumbosacral region
4 Sacral region sacrococcygeal (sacroiliary) region
5 Pelvic area femoral, pubic area
6 Lower limb
7 Upper limb brachioclavicular, sternoclavicular region
8 Rib cage costal-cartilaginous, costovertebral, sternocartilaginous region
9 Abdomen and others
M99.0 Segmental or somatic dysfunction
M99.1 Subluxation complex (vertebral)
M99.2 Stenosis of the neural canal with subluxation
M99.3 Bone stenosis of the neural canal
M99.4 Connective tissue stenosis of the neural canal
M99.5 Intervertebral disc stenosis of the neural canal
M99.6 Bone and subluxation stenosis of the intervertebral foramina
M99.7 Connective tissue and disc stenosis of the intervertebral foramens
M99.8 Other biomechanical disorders
M99.9 Biomechanical disorder, unspecified