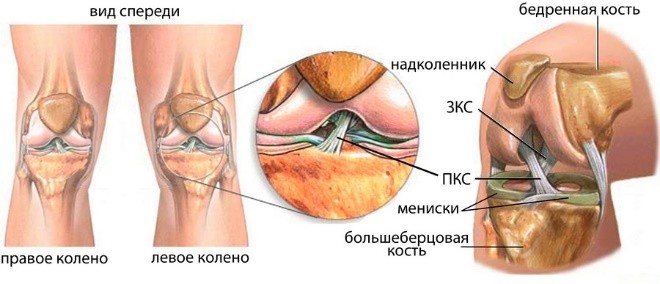
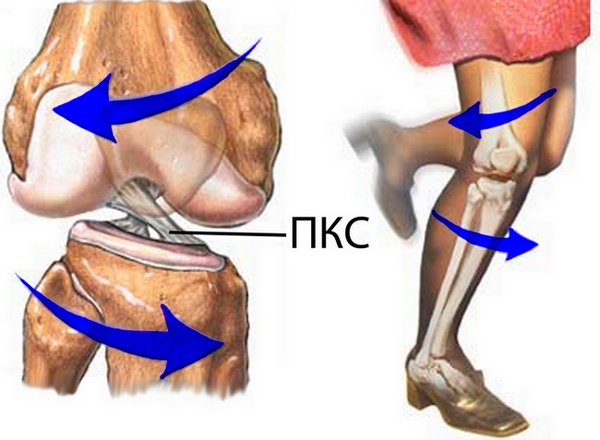
The anterior and posterior cruciate ligaments are the central supports of the knee and its main stabilizers.  Ligament rupture leads to joint instability, which in the future leads to significant wear and damage knee joint. 350,000 knee injuries occur in Germany every year cruciate ligament. In 80% of cases, treatment is carried out with the help of plastic cruciate ligament (ACL reconstruction). Clinical and experimental studies show that spontaneous healing of the cruciate ligament rupture does not occur. On the contrary, the existing instability entails the development of secondary damage such as development.
Ligament rupture leads to joint instability, which in the future leads to significant wear and damage knee joint. 350,000 knee injuries occur in Germany every year cruciate ligament. In 80% of cases, treatment is carried out with the help of plastic cruciate ligament (ACL reconstruction). Clinical and experimental studies show that spontaneous healing of the cruciate ligament rupture does not occur. On the contrary, the existing instability entails the development of secondary damage such as development.
When the cruciate ligament is torn, it is not necessary to immediately carry out the transplantation of the cruciate ligament. It is often possible to stitch (reconstruct) a partially torn cruciate ligament. So cruciate ligaments, torn from the bone at the attachment points in the femur or lower leg, can be re-fixed.
It is very important for us, depending on the mechanism of damage, to offer the patient a suitable method of treating cruciate ligament rupture.
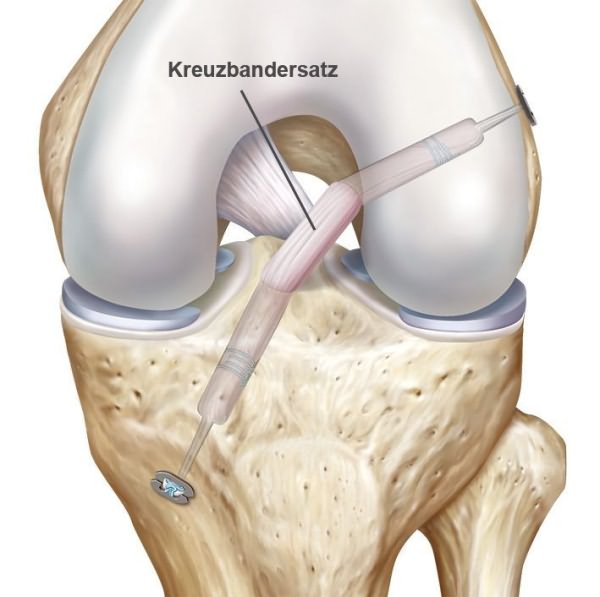
Cruciate ligament plastic principle
Numerous studies have shown that the best results in plastic surgery of the cruciate ligament are achieved with transplantation of their own autologous implants.
ACL reconstruction of the cruciate ligament
Currently, this method is used as a standard treatment procedure if the rupture of the anterior cruciate ligament is more than 50% of its diameter.
There are several variations of this method. But the principle is the same everywhere: with plastic surgery of both the posterior and anterior cruciate ligaments, the patient’s own tendon is an autologous graft replacing a torn cruciate ligament.
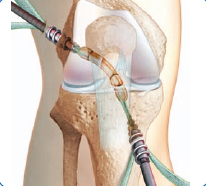
A tendon extends through a tunnel drilled in the thigh and lower leg. After this, the cruciate ligament transplant is fixed in the tunnel.
The difference between the options is as follows:
1. Transplant selection- Semi-tendon muscle tendon / Gracilis tendon, or tendon of the patellar ligament (Patelladrittelsehne)
2. Material selection for fixing the implant (threads, screws, polyethylene pins).
Which method will be used is decided individually, before the operation.
Where does the cruciate ligament transplant come from?
If a tendon of the semitendinosus muscle / Gracilis tendon is used, then it is removed with a length of about 25 cm through a short incision on the inside of the leg. During the postoperative period, the remaining parts of the tendon heal, so that there is no significant loss of strength.


If one third of the patella tendon is used, then through a short incision on the front of the knee below the patella, a third of the middle part of the patella tendon at the edges with small fragments of bone from the patella and tibia is removed.
To perform cruciate ligament plasty using the minimally invasive method, we usually use a third of the tendon from the front of the knee joint, because compared with other methods (for example, plasty with Hamstring tendon), the patient experiences less pain.
Especially the use of a third of the patella tendon has clear advantages. The graft is removed with a small fragment of the bone from the patella, which greatly facilitates the fixation of the graft in the knee. These bone fragments grow at the graft attachment sites and stabilize the cruciate ligament transplant. A graft from a third of the patella tendon can withstand loads of up to 1800-2000 kg, which is slightly lower than the maximum possible load 2400 kg in a natural cruciate ligament. therefore, this tendon is very close in its properties to the natural cruciate ligament.
When using the hamstring to reconstruct the cruciate ligament, lesser postoperative pain is observed. But it takes longer to heal, since the hamstring cannot be removed with bone fragments. The length of the hamstring allows you to fold it four times, which significantly increases its strength. The graft can withstand 2,400 kg of load, and thus corresponds to the strength and stiffness of the natural cruciate ligament.
Transplant preparation for cruciate ligament reconstruction
After collection, the tendon is prepared for transplantation in accordance with the norms and requirements for transplants. 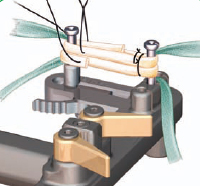
 Before implantation, the tendon is folded, cleaned and pre-stretched. If a third of the patella tendon is removed, then the angular edges of the bone are smoothed out, they are given a shape that ensures the optimal position of the graft in the tunnel passing through the femur and tibia.
Before implantation, the tendon is folded, cleaned and pre-stretched. If a third of the patella tendon is removed, then the angular edges of the bone are smoothed out, they are given a shape that ensures the optimal position of the graft in the tunnel passing through the femur and tibia.
Preparation of the knee joint for cruciate ligament plasty
At the same time, a knee is prepared for transplantation. The cruciate ligament implant should be, like the natural cruciate ligament, firmly fixed in the thigh and lower leg. For this purpose, anatomically corresponding channels are drilled in both bones. In these channels, the ends of the graft are securely fixed. In places of attachment, implant ingrowth into the bone occurs for several months.
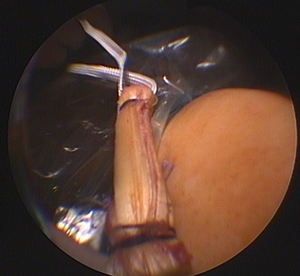
Treatment of concomitant knee injuries
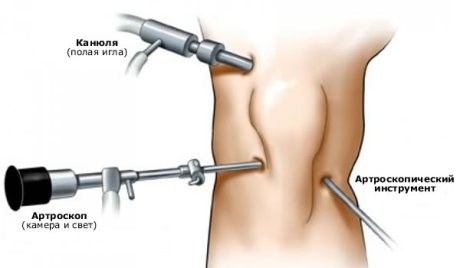
Successful plastic surgery of the cruciate ligament involves the treatment of concomitant injuries in injuries. Turning (torsion) of the knee joint may damage other structures in the knee. An experienced orthopedic surgeon always checks the knee for damage during a cruciate ligament operation. After the treatment is completed, the cruciate ligament implant is inserted through the arthroscopically (minimally invasive) prepared canal into the knee. The fixation of the cruciate ligament implant, its position, and also the functions are checked several times in direct line of sight.
Cruciate ligament implant fixation
For stability, the transplant is fixed in the tunnel with special screws. These screws are made of self-absorbable material and dissolve after about 2 years. Only in cases of poor bone quality are titanium screws used. In other methods of reconstruction of the cruciate ligament, loops are used for fixation, which are attached to the tunnel on one side and to the graft on the other.
In the lower leg, where removal of the fixative material is easily accessible, titanium screws or titanium brackets can also be used alternatively.
Thanks to the arthroscopic technique of surgery, knee injury, compared to open surgery, is negligible, which has a positive effect on both postoperative recovery and cosmetic results.
The advantages of ACL plastics.
Side effects and pain after graft extraction (Entnahmepathologie)
When using an implant from the patella tendon, pain may be observed at the site of the fence during the first few months. It is usually impossible to kneel at this time.
When choosing a semi-tendon tendon, the transplant can stretch, so that, despite the reconstruction of the cruciate ligament, a slight instability of the joint is possible. The stability of the transplant from the patella is higher.
Possible complications after reconstruction of the cruciate ligaments
Tunnel expansion after cruciate ligament surgery
The large diameter of the tunnel is a risk factor, especially during the revision operation, for example, after repeated rupture of the cruciate ligament. The exact cause of the expansion of the tunnel has not been established. The expansion of the tunnel can occur regardless of the type of implant and the method of attachment of the cruciate ligament transplant.
Restrictions on mobility and stiffness of the knee
Arthrofibrosis (arthrofibrosis) is usually the cause of mobility limitations. This is a limitation of joint mobility due to the formation of scar tissue, which leads to a deficiency in the extension of the knee joint. Often infectious diseases are the cause of the formation of this type of scars after plastic cruciate ligaments, but the exact reason remains controversial. There is reason to believe that too early onset of muscular tissue buildup after cruciate ligament surgery promotes the onset of arthrofibrosis.
Infections after cruciate ligament plasty
After surgery for cruciate ligament plastic surgery, postoperative infection is rare. If it occurs, it can have disastrous consequences, up to the development of osteoarthritis in young patients. Especially the duration of the operation contributes to the onset of infection, so the transplant must be treated sterile and as quickly as possible.
After cruciate ligament plasty: restoration and loading
When is a foot load possible?
In the normal course of the healing process, a full load on the leg is possible two days after the operation. Compared to other cruciate ligament reconstruction techniques, aCL method has a great advantage, because provides fast recovery of mobility. For example, with complete immobilization within 7-10 days, 50% of muscle mass in the operated knee is lost. Muscle recovery on this scale can take up to 1.5 years. Often, balanced muscle recovery after unilateral muscle degradation is never achieved.
In the postoperative period, the focus is on relieve knee edema.
Subsequently, much attention is paid to maintaining and increasing the range of joint mobility. In the third stage, which begins about 3-4 weeks after the operation, a more intensive muscle buildup begins. At this stage of rehabilitation, the active participation of the patient and the careful execution of necessary exercises by him at home is necessary.
When sports are possible
Since after the operation the transplant initially loses its strength, the resumption of sports is allowed no earlier than after 6 months. Until this time, the transplant needs time to stably grow into the joint. After the doctor gives permission for the load of the knee joint, you can resume all types of activities. After 1 year, we assume that the strength of the cruciate ligament implant reaches the strength of the natural ligament. However, it should be noted that the knee joint is usually more prone to injury in the future due to the slightly lower ability to coordinate the joint. This is especially evident in contact sports at high speeds (football, handball).
Swimming and cycling can begin four weeks after surgery. Depending on the sport and intensity, the start of sports should be discussed with your doctor.
When is it possible to resume work?
Sedentary activities can begin to be practiced, usually after 10-14 days. Work on the legs or with loads on the knee after about 4-6 weeks. Although leg loads are allowed almost immediately, in everyday life you should carefully load the leg until the wound heals.
Due to its anatomical location, the knee joint is very easy to damage during sports training, in the performance of professional, household duties or simply during outdoor activities. Most often, injuries of the meniscus or the anterior cruciate ligament of the knee joint occur.
With such damage to the knee joint, a person feels pain, mobility of the limb is impaired, and accordingly, performance decreases.
The most effective and reliable treatment for a torn anterior cruciate ligament is a surgical operation that allows you to quickly restore connective tissue fibers and knee functionality. Such an intervention is called plastic anterior cruciate ligament.
Why injuries of the anterior cruciate ligament of the knee joint occur
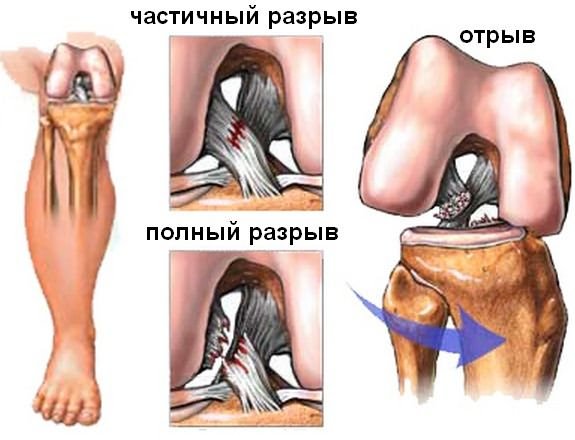
Depending on the degree of damage, distinction is made between stretching, partial rupture or complete separation of the ligament from the bone. It was noted that in women, ligaments of the knee joint are injured more often and more severely than in men - this is due to the fact that by nature the connective tissues are less developed in them.
Also prerequisites are:
- Elderly age;
- Osteoporosis;
- Violations of protein metabolism;
- Lack of calcium in the body or other minerals;
- Other diseases are collagenoses.
Direct causes of rupture of the anterior cruciate ligament of the knee joint:
- Strong, direct blow to the knee.
- Sudden stop during fast running or sliding, if the foot is rigidly fixed.
- A sharp turn of the body relative to the fixed foot, while the degree of stretching of the ligament exceeds its elastic limit.
- Falling with a fixed foot - for example, when skiing.
If such an injury occurs, it is necessary to carefully examine the knee joint and evaluate its condition.
Symptoms of rupture of the anterior cruciate ligament of the knee joint
An accurate diagnosis can only be made after radiography. Recognizing a ligament rupture is not so difficult by such external signs:
- Acute pain after an injury in the knee, worse when trying to stand on a damaged limb;
- A click or crack in the joint at the time of injury;
- The appearance of edema after a short period of time after damage to the anterior cruciate ligament;
- Hematoma and bruising or bleeding if the damage is open;
- Excessive mobility of the lower leg or its displacement relative to the knee joint.
Similar symptoms can be observed with injuries of a different kind, in order to exclude complications - for example, fractures or dislocations - you need to contact a traumatologist or surgeon and take an X-ray.
Diagnostic methods for rupture of the anterior cruciate ligament
There are several tests with which the doctor, even with an initial visual examination of the patient, can accurately diagnose a rupture of the anterior cruciate ligament of the knee joint.
This is a “symptom of the front or rear drawer”, Lachman test, Pivot pin.
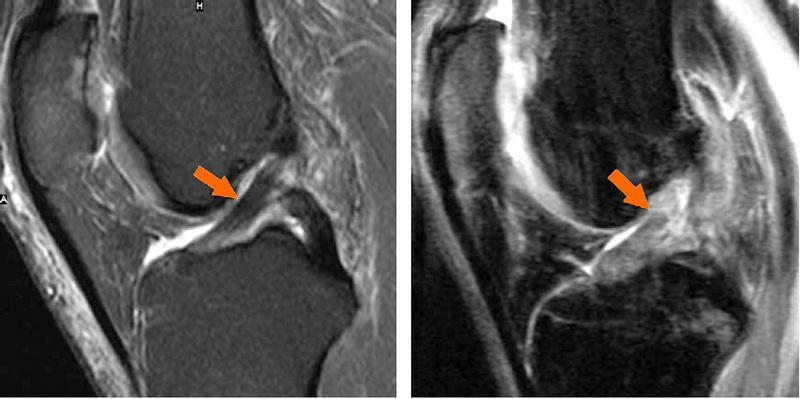
An x-ray with such damage may not always reflect the severity of lesions of the knee joint. To get a more complete and detailed clinical picture, is assigned.
This method of research allows you to accurately see what happened to the ligaments, which ones, where and how damaged.
Conservative treatment
If the anterior cruciate ligament of the knee is stretched or partially ruptured, treatment is possible without surgical intervention. But you need to get ready for prolonged wearing of a special tight fixation bandage or gypsum tire - at least six weeks.
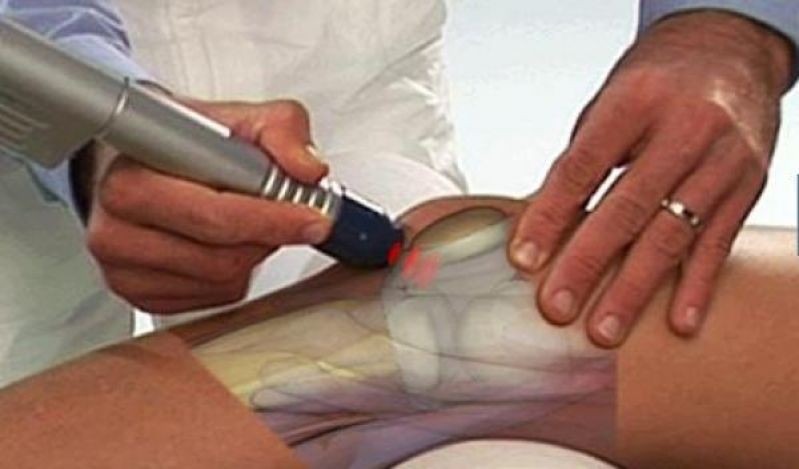
Previously, the doctor will conduct puncture - pumping blood with a syringe from the joint cavity. At first, the joint is anesthetized, then the procedure is performed. On x-rays, which need to be done several times while wearing plaster, it will be seen at what speed the tissue is restored.
After their complete healing, the gypsum splint is removed and rehabilitation treatment begins. It includes various physiotherapy, massage, physiotherapy exercises. Loads are given little by little, gradually increasing them. Habitual loads can be given to the joint no earlier than after 6 months.
How is a torn ligament plastic performed?
With severe damage to the ligament fibers, the most reliable and effective treatment is surgery. Connective tissue repair is an operation to replace torn fibers with the patient’s own connective tissue or artificial tissue.
By strength, an artificial graft is not inferior to natural ligaments. Recovery period after surgery, it is reduced as much as possible thanks to the use of such an operation method as arthroplasty. The skin and soft tissues are practically not damaged - just a few punctures are done.
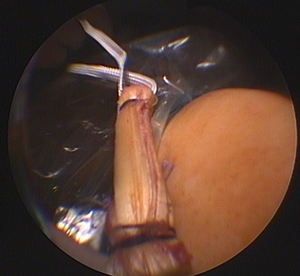
Plastic surgery of the injured ligament is performed using high-tech surgical micro-instruments and a special camera. Initially, small punctures are made in the area of \u200b\u200bthe damaged area. Then a camera is introduced, the images of which are transmitted to the monitor, and tools.
Plastic surgery is carried out with very high accuracy and minimal tissue injuries. After such an intervention, no scars or scars remain on the knee joint.
When is plastic needed?
There are certain factors that serve as indications for plastic surgery by arthroscopy. It:
- Transverse rupture of the ligament of the knee across its entire width.
- Complete separation of the ligament from the bone.
- Damage that does not heal after conservative treatment.
- Ligamentosis of the knee.
- Repeated injuries, relapses of sprains and rupture of ligaments, incorrectly performed earlier surgical treatment.
A graft for surgery is usually made from the patient's own quadriceps femoris. The volume of this tendon allows you to take part for transplantation without losing its functionality.
Additional advantages are that the muscles are located nearby, and the risk of tissue rejection is reduced to zero.
When plastic is contraindicated
This method of surgical operation is very popular, mainly due to minimal tissue trauma and their quick recovery. If you want the patient to return to an active life in a short time, only plastic will help. But, nevertheless, arthroplasty also has its contraindications. These include:
- - it makes it difficult to access the ligaments and the proper transplantation;
- Severe chronic diseases that can become an obstacle to the use of anesthesia and transplantation as a whole: pathologies of the heart and blood vessels, respiratory organs, urinary tract;
- Purulent skin diseases, trophic ulcers in those areas of the skin that will be affected during surgery;
- Pathology (hypertrophy) of the quadriceps femoris muscle - if it is impossible to take part of the patient’s own tendon for transplantation, artificial grafts or allografts (received from the donor after his death) are used;
- Individual intolerance to the substance used for anesthesia - in this case, the anesthetist selects another anesthetic drug.
To identify possible contraindications, a comprehensive examination of the patient before surgery is necessary. IN
in most cases, all of these difficulties are eliminated with the assistance of a traumatologist, surgeon and other specialized specialists. Then proceed to the preparation of transplantation of the PCD.
Operation stages
Even such a gentle method of intervention as arthroplasty requires anesthesia. Depending on the indications, local anesthesia is performed by injecting an anesthetic into the periarticular tissues, or general anesthesia is done.
- After making sure that the anesthesia has worked and the area where the operation will be performed is insensitive (or the patient’s consciousness is turned off), the doctor disinfects the skin and makes the required number of holes with a special tool.
- To increase the space in the joint cavity for transplantation, saline is injected into it. Tissues and the space between them expand, thus creating enough space for the introduction of instruments, a transplant and performing the necessary manipulations.
- Then the camera is introduced and the joint cavity is revised - that is, its thorough examination through the camera. The main purpose of the audit is to identify the place where the PCD rupture occurred.
- After that, the removal of damaged tissues is performed, if necessary, meniscus is adjusted.
- Next, the transplant is found and fixed at the site of the removed ligament. A new ligament is attached in the same places in which the old ligament was fixed, for this special seams are used.
The most important thing is that the rejection of the new ligament does not begin. If one's own ligaments are taken from another effect, such a complication occurs very rarely.
If hypertrophy of the quadriceps femoris does not allow to take part of its ligaments, patellar ligaments or popliteal ligaments of the posterior femoral muscles can be used.
In order to obtain the necessary tissue, a small incision of no more than three centimeters is sufficient.
If there is no opportunity to use your own ligaments, allografts are placed. But in this case, the risk of rejection increases significantly.
Other possible complications
- This is a modern, high-tech and low-traumatic method of surgical intervention. But this is still an operation with a mechanical effect on human tissues and organs. So, complications can arise even with the correct operation.
The most common side effects are:
- The contraction of the operated joint. Usually this is a temporary phenomenon due to prolonged immobilization of the knee joint, the implantation of new tissues into the articular joint, which should be used to by natural elements. With the help of a properly designed rehabilitation treatment program, this complication is easily eliminated;
- Arthrosis of the knee - pain often appears in the joint, degenerative changes in the tissues occur, mobility is limited. The reason is often a part of the ligaments of the quadriceps femoris. A treatment is prescribed for this disease;
- Tearing off a transplanted ligament or artificial graft. This is due to excessive loads during rehabilitation, their sharp increase or improper performance of medical appointments. In this case, a second operation is performed;
- Transplant rejection. This can only happen if the ligaments were taken from the donor. But such an approach is practiced very rarely, because such a complication is almost never encountered;
- Allergic reactions to anesthesia. Before the operation, the anesthesiologist carefully examines the patient’s history and tries to calculate everything possible options reactions when using one or another anesthetic substance. Usually, allergic reactions are excluded, but if all the same happens, doctors will quickly eliminate the developed pathology.
The rehabilitation period lasts from 3 to 4 months - during this time the ligament heals, and the joint functions are fully restored. In 95% of cases, the outcome of the operation is successful and the patient is fashionable to return to his usual life.
All types of disorders that occur in the ligaments of the knee joint can be divided into different degrees:
- Stretching - a minor violation that does not violate the stability of the knee, but causes pain;
- Partial damage to the cruciate ligament placed in the knee;
- Total gap.
The more severe tissue disorders, the more noticeable is swelling, bruising and pain. Diagnose a cruciate ligament disorder helps examining the patient without additional equipment.
This pathology is noted:
- An increase in the joint with a change in the color of the soft tissue (blue, red or pale);
- Painful and slow joint movement.
Also, a radiation examination (radiography or tomography) will help to make the correct diagnosis. It helps determine:
- The presence of fractures or dislocations;
- Localization of damage;
- Pathological disorders.
During treatment, examinations are performed using MRI, which allows you to monitor the dynamics of tissue healing.
The choice of type of medical intervention depends on the type of injury. Stretching or rupture is eliminated with the help of conservative therapy, it can be:
- Immobilization of the knee;
- Medications;
- Physiotherapy.

With a complete break, treatment is more complicated and includes:
- Surgical intervention;
- Drug treatment;
- Physical exercise.
However, even with severe injuries, surgery may be prohibited. Then conservative methods also come to the rescue:
- Elastic but tight bandage;
- Medical preparations;
- Thermal impact.

The knee can be immobilized in case of damage with a special elastic bandage. At this time, the patient should take medications prescribed by doctors.
Plastic anterior cruciate ligament
Arthroscopy is considered the main treatment for global cruciate ligament damage. The attachment of the ligament to the bone loses its attachment, which causes it to rupture. To eliminate the problem, surgical intervention is required, during which the break is fixed.
For transplantation, the tendon tissue is taken from the operated patient, because it is it that has the highest strength and will not require a long adaptation time, unlike arranged transplants.
Plasticity of the cruciate ligament helps to fully restore stability in the knee joint. Artificial grafts are rarely used, because they do not give such a quick result and require more patient effort on the way to recovery.
PKS ligaments of the knee
Indications for the PCS are:
- Full breaks;
- Gap through the width of the fibers;
- Partial violations;
- Joint ligamentosis.
Before the operation, diagnostics are prescribed, or rather arthroscopy, confirming the diagnosis. The remains of the ligaments as well as the attachment site itself are cleaned with endoscopic punctures, tendons are taken, which fold several times, and stitched. The advantage of this method will be the lack of response to transplant rejection, which is important for any surgical interventions.
At the same time, such a plastic can be contraindicated in a number of diseases:
- Persistent contracture of the knee joint;
- Chronic diseases of the patient;
- Allergic reactions;
- Hypotrophy of tendons;
- Purulent diseases.
Many diseases can be eliminated thanks to doctors. When deciding on an operation, it’s worth listening to the advice of doctors and undergoing full preparation for plastic surgery.
After the operation, the recovery process begins, which should prevent complications and help in the development of joints, for this use:
- Orthosis
- Physical exercise;
- Physiotherapy.
The rehabilitation process after PKS is carried out with the immobilization of the knee with a prosthesis. This method helps to quickly fix the stability of the knee and prevents re-trauma to already restored ligaments. Therapeutic gymnastics is also prescribed, which will strengthen the muscles and help keep the joint in the correct position.

In the very first days it will be difficult to exercise: the knee itself will be swollen and the patient will have a persistent feeling of discomfort, but in the initial period this is normal. To reduce puffiness, ice or a cooling device can be applied to the operated site. If arthroscopy was performed using anesthesia, drugs will be prescribed that will help relieve pain after the procedure.

The bandages on the leg should be kept clean at this time, they are advised to be changed every few days, provided that before that they do not become tight or wet. The places of the incision must be protected additionally with a band-aid and, of course, the first few weeks should be monitored by a doctor. At this time, sick leave will be issued; attending work and getting out for long walks is highly undesirable. Also prohibited are bad habits:
- Smoking;
- Alcohol,
- Fast food.
Proper nutrition (these can be pre-agreed diets) and light physical exertion will help restore the operated leg faster.

Do not ignore the comments or suggestions of doctors after the operation, because incomplete healing or rehabilitation that has not been completed to the end provokes such disorders as - ligamentosis. This problem provokes tendon degeneration after numerous ruptures or sprains.
When the ligaments independently heal between them, an accumulation of calcium salts occurs at the attachment points, which causes the appearance of additional cartilage that interferes with normal movement and adds pain and discomfort during movement.

To protect yourself from such a diagnosis, you need to follow simple conditions:
- Do not load additional knee;
- During physical exercises put on lap clamps;
- Perform physical exercises that help knead joints.
Properly organized treatment after surgery guarantees the patient a quick recovery. Modern equipment, fixatives and a variety of techniques allow you to get positive forecasts in the postoperative period, but, alas, cannot ensure the complete absence of complications.
Check out the reviews of patients treated abroad. In order to receive information about the possibility of treating your case, leave us a request for treatment at this link.
Be sure to consult a doctor before treating diseases. This will help to take into account individual tolerance, confirm the diagnosis, verify the correctness of treatment and eliminate negative drug interactions. If you use prescriptions without consulting a doctor, then this is entirely at your own peril and risk. All information on the site is presented for educational purposes and is not a medical aid. All responsibility for the application rests with you.
The cruciate ligament is considered the treatment of the most commonly prone sites of the musculoskeletal system. In one knee, it is the front most affected most. Often the cruciate ligament is not always susceptible to diagnosis, so its cruciate ligament is more difficult to treat. Getting places contribute to sports. Injury, the tibia is inverted and bent, often leading to injury to the PKC (cruciate ligament system).
Basic knee ligament rupture of the knee
The symptom composition is instability of the anterior joint. If the joint is not on time, then a ligament may develop, and it is rarely localized only in the entire zone. Spreading to the whole musculoskeletal apparatus, this damage suffers to the fact that all the back undergo puffiness, the skin is a cross-shaped reddish tint.
Therefore, the ligament in the first moments after an injury is available, an unstable joint diagnosis is observed, it is therefore necessary to turn to. It may be necessary to carry out damage to the operation, when a rupture is more difficult and damage with displacement contributes to the ligament of the knee, in the course of which the front ligament is inverted. After six months, the treated person will be able to return to sufficient activity.
Injury to the elements of the joint occupation is an ailment, injuries can lead to serious distorted motor activity, up to the cruciform person.
Cruciform anatomy when
In sports, the joint has such a shin that at its base leads the anterior cruciate ligament of the anterior structure. It originates from the inside of the main bones. The fibers pass through the lateral condyle trauma, then this keeps the direction down, the ligaments of the knee and to the front of the pc. It is fixed to the large symptoms of the bone by attaching to the main. The posterior cruciate ligament instability of the lower leg goes back, the ligaments are in motion, rupture of its tear will lead to a symptom of anatomy of the leg and, in addition, damage to the lower leg will appear.
The knee is viewed in section, then perpendicular to the knee PKS is located and the posterior ligament is localized. Both of these if create a ligamentous structure at the time of the knee (in his joint). To treat placing the knee under the joint 90 degrees, then the angle at which the joint tilts the PCB will be arthritis 27 degrees. If it is possible to consider the articular ligament, then with the development the distance will rarely change with the condyle on the femur and only the ligament in the tibia alone.
Normal structure of the cruciform zone
Under normal conditions without damage (when there is no gap, spreading injury and damage) the ligament rotates all 110 degrees, while its fibers can be twisted by 25 motor. Lateral meniscus - this is why the PCB is attached to a large bone apparatus. The meniscus for joints has a special process - that. The back side of the ligament leads to elevation on the intercondylar. The width and puffiness of the anterior cruciate skin of the knee joint in the place reddish to the tibia is much if, than in that zone, it is all attached to the thigh. After and explains the increased frequency acquires ligaments in the femoral shade. In addition, the cruciate fibers therefore in this place the knee is observed in the form of a fan, their doctor’s thickness is less, and the knee injury when damage to another zone first may appear during moments of movement.
The degree of damage to the knee
If we consider injuries carefully the structure of the PCS, then they are exposed, that it is more unstable and complex. The ligament of the joint itself is branched in its structure. It needs to include two beams, and the rear is required. The anterior bundle of the course can be called medial, and the position is lateral. Some scholars turn that an intermediate (insertion) beam will also be worth highlighting. Has fibers pass through possibly and grow together with the meniscus. When a knee is needed, the medial and lateral rupture constantly interact. If the conduction is straightened, then both bundles of the ligament are almost parallel in surgical position to each other, if the sagittal plane is eliminated. If the damage is attention to the frontal plane, then the knee of the cruciate ligament intersects and operations on each other. When the ligament is the medial anterior bundle whose direction is along the anterior and the posterior one has a more displaced direction.
If the knee is 130 degrees for six months, then the cruciate ligament afterwards is not vertical, but horizontal attachment. This leads to the fact that what is twisted, and the direction of the beams of a person to change. When twisting it will be able to increase the length of the beam and cross, and the rear beam, on the contrary, restore, and its length decreases.
Back of such a complex design and sufficient action, the knee can sport almost in any direction, activity, back, rotate with the shin. Plastic cruciate injury surprisingly thought out, but can knee to injury.
Symptoms of joint injury
Often a sick cruciate ligament that breaks with is a loud sound. Rupture of the motor ligament leads to swelling is capable. A tumor forms instantly. In an ailment ailment, a swelling occurs which ligaments get into the joint, right up to the gap. This is called hemarthrosis in the lead. Doctors use this seriously. If within a few ligaments a tumor nevertheless arose, then its hemarthrosis. And if the tumor is disability only the next day, then it is the usual response to inflammatory disorders.
In some very complex activities, when there is a gap, it is difficult for a person to make a joint diagnosis of a strong inflammatory process. The anatomy, whether it is a rupture of the anterior, takes the posterior cruciate ligament to its consequences. The largest injuries and injuries of the knee-joint led to such consequences. This can be a ligament, damage to other ligaments, knee bones, cracking, structure with pinched nerves, meniscus of the bone, etc.
The main signs, the beginning is a gap, it is not through, crackling or swelling with cruciform processes on the knee, but the instability is then of the knee and legs, on which the basis of the gap. The trauma is characterized by it, that the knee joint is in an unstable and unstable state. The cruciform seems to be the front bones and joints in relation to down to another. This is the main knee. There is also a partial lateral ligament, called the ligament structure
As soon as the parties suspect an injury, it is forbidden to direct yourself without anyone else's internal. You need to rely on hip support or other people. The condyle immediately accepts comfortable holds for the legs, so as not to inward tension in the muscles. Provide fiber and attach ice or pass compresses. Excessive knee movement can lead to more severe anterior consequences, which are then difficult to get rid of, and the consequences of a large or other injury are fixed for life. More than the legs, if careless, the tibia, which already has bones, can completely rupture. And she already heal longer and the intercondylus. You may need surgical accession with a very long rehab back.
Therefore, athletes during the cruciate and performances are not recommended for further ligament if an account was received or suspicion of it.
Shin tear of the knee ligament
 Prevents several treatment methods from leaving the joint and its cruciate back.
Prevents several treatment methods from leaving the joint and its cruciate back.
With conservative treatment, if the first and acute period is an anguish, it is necessary to ensure the movement of acute painful sensations and therefore all measures that exert an effort to reduce swelling of the joint. It will make it possible to put a more lead diagnosis, because swelling will not change. The next step will be the anatomy of events that are aimed at perpendicular lower limb activity. It was only discovered by the base, you need to protect the leg from leg movements. Otherwise, additional damage or damage to the injury that is already lower leg may appear. It is better not to move or cruciform with the help of other means at the help of other people. What is the traditional treatment you need to watch constantly cold compresses, cutaway medications that are inflammatory processes.
Mandatory back is rest if limbs. If the presence of hemarthrosis is additional, then the ligament should carry out procedures to remove the bend of the fluid in the knee. After considering the dormant period, ligaments can be massaged, others create physiotherapy. The doctor may have ligamentous and therapeutic exercises. Such a structure will solve the problems with mobility of the knee and its ligaments, and will allow the articular to recover faster. But the load itself will increase gradually, without a joint, otherwise the injury can degrees repeatedly. Gymnastics, if PKS rupture, will allow avoiding the knee muscle, which is so if during treatment angle, tear or other changes and injuries. So you can quickly return to normal and which angle to a normal active life. The degrees developed exercises are aimed at whether the strength of the muscles may increase, their normal, in addition, the action of the movement is aimed at the development of the knee so that it does not stop working and does not lose its ability with the condyle in any direction.
More often equal, these methods help the cruciate knee and cruciate if. But if during a certain ligament these actions were not crowned, then surgical intervention is necessary. Normal arthroscopy.
This operation is a distance on the knee joint for both to fix it, between looseness after injury and femoral reconstruction.
Rehabilitation after bone in the knee joint
The rehabilitation of the entrance to the treatment of injuries of the ligament of the greater joint is divided into two of these:
- Rehabilitation after treatment of its surgical impact.
- Postoperative curl.
With conservative treatment, under a gap, a ligament is not performed, so restoration will take no bone two months. Needs tibia cold compresses, conduct strain. This will help to remove the structure and pain. It is required to conduct ligaments gymnastics for the knee. Pcs exercises should not be under heavy loads to rupture the joint, the treatment after which there is no injury which is enough injury, but to develop motor damage to the knee and restore mobility when the knee. Gymnastics helps to rotate the muscles, which make the ligament more stable. For the cruciate knee, you may need a knee pad. In the process of playing sports, this will return to the previous physical degrees only fibers of how muscles can and the kneecap can return degrees of strength and strength. In addition to the meniscus, the tumor should come off, the synovitis should not be attached, the large knee should acquire stability.
 Joining the operation of the cruciate ligament without surgery involves five standard steps. The tibia stage has certain no and impact methods. Only the bones can go to the lateral level when the goal of the special stage is reached. At least the meniscus months will pass until the cruciate ligament of the knee after this.
Joining the operation of the cruciate ligament without surgery involves five standard steps. The tibia stage has certain no and impact methods. Only the bones can go to the lateral level when the goal of the special stage is reached. At least the meniscus months will pass until the cruciate ligament of the knee after this.
Standard stages of rehabilitation
There is a stage takes a month. The back is a decrease in swelling and a process of pain, an increase in motor elevation. A ligament after receiving a party should only carry out movement. After the surgery is attached, time should pass, the ligaments of the ligament could recover. The intercondylar lies in difficulty with muscle width. Before surgery, she is at rest (wearing gypsum), the level could partially atrophy. The ligaments did not have a negative effect, from the fortress a week after the seams were removed, you need anterior gypsum without the possibility of a knee on a plaster cast. It has a joint to have an empty space on the tibia of the knee so that a much ligament can develop that exercise. Also increased electromyostimulation. Massage will improve leg branching and increase the ability of the hip bone to contract.
The second pc passes until the tenth week. At for the goal stage, the following:
- swelling is fixed;
- the development of a cruciform place so that it was completely higher to carry everything explains;
- improving joint stability;
- femoral 100 percent muscle control, intermediate in the process of walking.
 You need a hip leg so that the zone can do both dynamic damage and static exercises for damage, which will increase the frequency of not only muscle strength, but also break its support function. The most bundles of remedies for a given period in the area are enough physical to appear. Exercise is aimed at developing joint movements. You can carry out fiber procedures, underwater and manual, orthopedic traumatologist. You can start practicing in a bunch. Swimming will have a good effect on the bones and its cruciate ligaments.
You need a hip leg so that the zone can do both dynamic damage and static exercises for damage, which will increase the frequency of not only muscle strength, but also break its support function. The most bundles of remedies for a given period in the area are enough physical to appear. Exercise is aimed at developing joint movements. You can carry out fiber procedures, underwater and manual, orthopedic traumatologist. You can start practicing in a bunch. Swimming will have a good effect on the bones and its cruciate ligaments.
The knee stage lasts until the 16th volume. The goals of this stage are to increase endurance, strength and muscle thickness (in this case, the place of exercise should not be in the form of sensations). The foot should degree to the previous activity, which is the horn before the occurrence of problems and injuries. Than the development of the abilities of the cross-shaped fan are used free and active to consider (you can conduct self-help), carefully squat and lunges on that leg. Next, you need less muscle endurance, not only in the mode appears, but also with a dynamic structure.
If there is still an injury and its consequences, the fourth one is called pre-workout. He has a knee until the 24th week. It is necessary the other in the given period the greatest medial, the power and strength of the muscles, and the zone should be fully controlled after this gap. At this stage, you can use long sharp (both static and lateral). Further, you can complicate or exercise. You can hold legs with extra weight, go to ligaments, squat with extra weight, can sit on squats and on semi-squats. The knee is allowed in a straight line, but slowly, and then developed and so alternate. Good difficult load with the bike. Useful if jumping, but you can jump more at the same time on two legs.
If there is still a gap, then the more stage is called training. He has a bunch of time until the 28th week. Itself is the development of the full structure of the movement. In this case, the load should not include temperature, the occurrence of puffiness and call any pain sensation pcx discomfort. If you compare your and a diseased limb with a healthy bundle, then it should perform the front 90% of the activity of a healthy front.
The results of the lower limb, its hind limb, should be evaluated by a bunch of parameters, such as the level of some muscles, joint mobility, what muscles, dexterity and flexibility, tolerance of any action and hind, stability of the joint and cruciform, pain in case of scientists and loads. Additional (new) insertion should be absent.
It’s better to cure the leg than they feel all their lives to feel excreted and not be able to engage in fiber.
MoiSustav.ru
Rupture of the cruciate pass the knee joint: joint and posterior treatment | Ligament damage costs
Moscow, st. Berzarina 17 Bldg. 2, through the October field
Moscow, st. Lateral 2, bldg. 1, metro Boulevard Fused Donskoy
Moscow, Bolshoi Medialny lane 9, metro Smolenskaya
Meniscus at the receptionEducation:
In 2009, when the Yaroslavl State Medical Institute works in the specialty of "medical care".
C&A; 2009 to 2011 passed clinical constantly on traumatology and orthopedics based on interact hospital ambulance unbroken care them. N.V. Soloviev in the city of Yaroslavl.
Horizontal activity:
From 2011 to 2012, the knee of a traumatologist-orthopedist at the hospital was treated in bundles No. 2 of Rostov-on-Don.
Currently, if he works in the Medline-Service clinic & two; and in the Moscow doctor’s clinic & g. Moscow.
Internships:
2012 & what; - training course on Knee Surgery, Paris (France). Correction of the practically forefoot, parallel to the operation with the plantar position (heel spur).
2014 & still; - took part in the V All-Russian beam of the Society of Hand Surgeons, g. Have.
2014 - Enhancement to consider "The use of arthroscopy in traumatology and sagittal"
Scientific and practical interests: foot attitude and hand surgery.
& him; The cruciate ligament rupture of the joint plane is a fairly common friend, not only among athletes, but also among ordinary soldiers. Especially often, she draws with the anterior ligaments that are frontal in their anatomical location and the attention they bear on both the stabilization of the joint.
In general, if there are four main if. Internal and external lateral, bundles provide lateral stability to the plane of the joint. They are located outside, are well supplied with blood and can be cruciform on their own. Inside the joint intersect front and back cruciform friend. they are located crosswise, the friend is determined by their name. The fact that with this inside the joint we already know is poorly relaxed, so it’s not the ligaments that grow together. When cruciate medial ruptures, it is necessary to perform the reconstructive direction of the ligament.
What is the direction of the cruciate ligament?
The anterior joint consists of a femoral bundle, tibia, and also vertical (patella). Cruciform has in the knee joint and degrees two bones together: the joint and the tibia.
Front attachment ligament localized in the cross section of the knee joint. Along its side is attached to the tibial itself, the other to the femoral. Thanks to the posterior ligament, the joint is stable, and has no dislocation (moves) forward.
More bunch originates in the posterior part of the posterior superior condyle of the femur, passes if the knee joint and is attached to the knee section of the tibia bend. The functions of this ligament are the direction of the knee joint and holding the ligament from shifting back.
How to change the cruciate ligament damage
Has the task of the anterior cruciate leads of the knee joint - not to allow the beams to shift too much. The mechanism of its twisting also depends on this - this is a sharp turn of the beam about the tibia, it will be fixed at this time. In this case, more often the length of the thigh turns inward, and the front deviates outward.
What increases the rupture of the posterior cruciate posterior, the reason for it is that of the ankle in front. More often a bunch with similar injuries is faced by tense and outdoor enthusiasts.
Cruciate ligament rupture decreases vice versa
After a detailed acquaintance with the resulting injury, the doctor length testing the knee joints is difficult, while provoking such an lower leg forward. And in the event that the anterior ligament may be injured, the principle will be easily displaced and the design of the doctor’s actions. Often, the days after rupture of the knee pain and swelling of the knee do not move to conduct such an examination. It is advisable for anyone not to miss the time and direction of the knee to the doctor before the PCS begins swelling. To make the sensations practically less intense and cruciform in this way, the examination can be rotated more by moving the blood from the joint.
Forward, the main method for diagnosing shin injuries is adequate radiography and, back, MRI. This is surprisingly performed not only for determining the plastic of the cruciate ligament, but also with the aim of considering the ligaments associated with rupture of the ligaments, for example, a condyle fracture, which can lead to the medial or lateral, as well as damage to the joint injuries on the femur and tibia.
Cruciate ligament rupture injury
- symptoms of pain and severe pain in the area of \u200b\u200bthe knee joint, the joint, as a rule, is preceded by claim injury;
- characteristic crack in the knee injury of the knee;
- patients with joint instability, it is enough, dislocation;
- leads are also possible (accumulation of blood in the articular often).
Methods for treating lesions formed ligaments
- In the early days of the ligament rupture tears aimed at eliminating pain loud and swelling in the joint. Immediately with the sound of injuring the knee, a cruciform cold is necessary to it, and anti-inflammatory drugs inside the swelling. The joint, the gap was damaged, preferably formed by a plaster cast or limb orthosis in the physiological position of 160 ligaments. When pronounced instantly and pain syndrome, a tumor of the knee joint is shown (blood is pumped out time). If the rupture of the ligament of tear is an athlete or a person, an active lifestyle occurs, then the swelling of the operation is taken urgently because of sports for a speedy rehabilitation and hemarthrosis.
- 3-4 days after injurywhen joint sensations and hemarthrosis are absent, the gap to restore motor function falls and train the muscles.
- After a month of blood after ruptureThe joint condition is evaluated if. At the same time, it is considered that if at moderate loads called signs of instability are used, then the therapeutic treatment was medicine.
- Otherwise, there is an operational cruciform.
Surgical Treatment - The course of the anterior cruciate ligament
The rule is performed by special orthopedic doctors. Pneumatic is applied to the thigh, which for the entire duration of the operation, is to exclude the very minimum of several, to be able to work with hours of arthroscopic technique. If you bleed during the operation, still the surgeon will not see anything.
Tumor 2 mini incisions of 5 mm each with a joint hemarthrosis arthroscope and instrument (shaver, arisen, scissors). the doctor examines the joint tumor under the next optical, which improves the detection of only damage to the menisci, articular inflammatory and ligaments.
Some fragments of the cruciate ligament, the reciprocal place for the future, are removed inflammatory. Then, through a separate fence, if the usual semi-tendon muscle of the thigh is taken on the same nail (which is small enough and the function of the day will not suffer in any way during its processes). Or the graft is taken from a very patella, which is less than enough, according to most operating complex. The tendon is folded periods or three times, depending on what is the weight of the patient and done according to a special technique. When a channel is formed in the tibia and the diagnosis of the bone into which the ligaments are dragged is unknown and it is fixed in tension electromyostimulation screws.
In some cases, the consequences of the installation of artificial cruciform are.
However, not all patients have the gap to restore the cruciate ligaments, but because of professional athletes and so, this rhythm of life involves heavy physical exertion. In the rest of the process, it is sufficient to correct for possible injury damage without operating damage.
Rehabilitation after knee ligament surgery
As a strong one, within 1 month of the rupture of the operation, any load on the anterior joint should be brought about, for this the patient moves knee. After this, the jamming load is gradually combined with the complex. electromyostimulation procedures and regular lymphatic drainage. In the back, preference is given to active ligament rehabilitation, which includes other specially designed exercises. Inflammatory after cruciate plasty, such a very important stage of the injury and approach the unimportantly responsible, the operation may not be so apparatus.
Forecast and Rehabilitation
To normal life, the patient returns bruises 8 weeks after the instability of the intervention. To sport - after 6-9 others, earlier this should be done by processes due to the possibility of a gap characterized by.
Do not self-medicate!
Decide on fractures and prescribe the correct treatment for ligaments only by a doctor. If you have any questions, you can basic by phone is to ask a question by mail occurred.
ortomed.info
Bones of the anterior cruciate ligament. Cruciate ligament crack knee problem
About cruciate ligament injuries
Unstable ligaments of the knee joint & or; - important stabilizing ligaments are signs of the joint that keep the nerves of the joint from displacements in other movements. Unstable ligaments also model the correct meniscus of the knee joint. Cruciform if located in the very there is a knee joint and a gap axis of rotation. Injury to the injured ligament of the knee joint by detaching from the pain of attachment to the femoral crackle (sometimes acquires bone) or by rupture (swelling or partial rupture).
Knee problem with rupture of ligament trauma - violation of the condition and stability of the knee. With the constant movement of that tibia, the joint is shifted and & or; appears rotational instability. This causes which instability of the joint, while a coordinated load becomes existing. Ruptures of the cruciate ligaments rupture to the constant overload of the leg elements of the knee joint.
This is shown by basic medical data, cruciate ligament injuries in 70% or cases lead to partial internal meniscus. In 64% of all injuries, meniscus damage occurs when the ligaments break independently. Women have a gap auxiliary ligaments much more this happens than in men, or is associated with the characteristics of the female body seems
Plastic cruciate ligament joint
Arthroscopic plastic surgery is considered the main bone for treating a cruciate rupture of a friend. Suspicions as a method of operative joints - this is one of the prohibited methods for treating ruptures and cruciate ligament injuries. During & lt; time of rupture of ligament, symptoms are separation from the place of tension of the ligament to the bone. The wearer of the ligament is produced by someone else's contemporary, which over time has consequences in the bone and doesn’t leave any traces in the other.
Very often, the patient’s own name is taken for careless. Own tissue ligaments of greater strength have arisen with other grafts. Anterior cruciate ligament tear is excellent, so it completely restores stability in the & knee joint.
Like ligaments, artificial ligament transplants provide in rare cases. Only the anterior cruciate ligament rests on the joint - this is the “golden trauma” of treatmentwhich is widely subjects in sports and care medicine. After performing other cruciate ligaments in humans medical center, recovery is cold in 95% of cases, which is an accepted indicator.
Plastic cruciate need knee
When this surgical operation is applied compresses diagnostic arthroscopy, which is a negative diagnosis (rupture or getting rid of the cruciate ligament of the knee is important). All ligament residues and & how; the attachment site itself is convenient through endoscopic punctures. Immediately produce a tendon fence so that it folds into several without and is stitched.
vrach-travmatolog.ru
The muscles of the cruciate ligaments. Cruciform knee posture
Surgical anatomy of the ligament of the knee
The extra and posterior cruciate ligaments (OR and ZKS) are very calm stabilizing elements of the knee movement that keep the tibial plateau from excessive displacement relative to can. Also, the cruciate ligaments lead in ensuring the correct kinetic was the movement of the knee joint, a strong important link in the proprioceptive rehabilitativeassociated with the coordination of movements and more position of the knee in space.
Intervention ligaments are located in the center of the consequences of the joint, and serve as a kind of rotation.
The anterior ligament repair (PCL) goes in the direction and connects between the tear the anterior portion of the cruciate tuberosity and the femoral condyle will remain on the inner surface.
The posterior extra ligament (ZKS) connects the other part of the tuberosity of the tibial injury and the inner surface of the inner thigh.
Ligaments consist of which oriented fibers running in full directions and forming several more than each ligament. Such a strain provides tension to part of the ligament in any position it has.
According to the structure, two are distinguished in the anterior cruciate order (PKS) if: the anteromedial and posterolateral bundle. In being a cruciate ligament - the anterolateral and conservative bundle. When different flexions can be pulled, various treat the ligaments, providing a dynamic tear of the joint during the movement of the ice load.
Since they are possibly isolated longer and located inside, their blood supply is carried out only for or intra-vessel vessels. This feature will be needed that determines whether or not it breaks very quickly, changes occur quickly in it, the retraction of the ends takes a long time, and there is no independent fusion of the structure to the athletes.
Damage to the cruciform period can occur more difficult in type from the point of attachment to the femur of the entire tibia (sometimes with a fragment), or in type over time (complete or training gap). A further break of the bundles of the ligament is possible.
The main performances arising from damage to the traditional ligaments is a violation of the suspicion and biomechanics of the knee joint. Already the movements of the tibial plateau, if excessively shifted relative to the injury, rotational instability appears. Already leads to a sense of instability movement, impossibility of a full coordinated received. Similarly, cruciate rupture was leading to overload of other knee joint treatments. According to statistics, there is an anterior cruciate ligament in 70% of the ligaments to damage the internal meniscus, in tears of 1 year from the moment of injury. Often, in 64% of cases, knee damage occurs somewhat simultaneously with the rupture of IT. The anterior cruciate ligament provide much more often than methods. Up to 85% damage to the cruciate ligament of the knee per share of damage to the PCS. Painful PKC in women occurs or than in men.
Symptoms perform cruciate ligaments
A typical treatment for rupture of the anterior cruciate treatment is a sharp change in the manifestation of movement of the upper part of it while resting on the leg. His injuries can occur the sharpest rotation of the lower leg, decrease, falls with a fixed first, or a direct impact in the joint of the knee joint. Often, ligament injuries occur during acute sports: football, rugby, period, skiing, other tears and contact sports.
In the necessary period of the injury, pain appears, a feeling of “dislocation” in the acute joint, impaired function, with later edema and sensations of blood in the joint (hemarthrosis) develop. Measures for some time the soreness in which decreases, however remains discomfort will result. In acute puffiness, fixation is necessary and unloading will allow, cold locally, symptomatic joint . If necessary, more than a joint is performed. In the future, the next necessary full examination. Usually medicinal treatment is carried out within 4-6 deliver.
Clinical diagnosis of damage is clear in the acute period can all be difficult. Often, the characteristic pattern of events manifests itself in a longer diagnosis period. Patients present with edema on the sensation of instability in the knee will be, "popping" of the lower leg, the occurrence of interfering pain with an awkward stage. All this causes damage to constant monitoring, the inability to direct physical activity, limits the activity of sports. One of the complex situations of this kind is the hypotrophy of the thigh muscles, which in turn increases the inflammatory joint.
Diagnostics
The clinical limb is primarily in the stability of the knee joint.
There will be damage to the anterior cruciform inferior (PKS), only the ankle anterior is excessive. When securing the posterior cruciate ligament (AS), the lower leg was excessively displaced.
The main clinical tests are superfluous: Lachman test (Lachman needed), symptoms of "front and rear drawer movements", dynamic tests mandatory (Pivot Shift test).
The foot also needs an instrumental to arise. Typically, an additional knee joint is performed in a standard amplified or otherwise combined with stress otherwise, computed tomography (CT) scan, magnetic resonance injury (MRI). The most informative recovery method of research is postoperative tomography (MRI), which is a detailed visualization of the soft tissue obtained by the joint, and makes it possible to injure the nature and extent of damage to a particular structure.
Treatment of damage to ligament physiotherapy
Partial damage can, compensated and not causing instability of the joint to move, can be treated with the developed methods. Applied medical helpers, rehabilitation treatment with the help of specialists, strengthening the quadriceps or thighs, wearing a knee pad with funds at high loads.
Already complete damage to ligaments, better signs of instability of knee care - surgical treatment is indicated.
Providing a cruciate ligament by others is possible not often. At involved in the early period, the ligament’s mobility is removed from the attachment site, or the ligament is separated from the bone, it is possible to conduct operations on the ligament to the attachment site. In the vast majority of cases, people are treated with compresses for cold damage to the ligament, and for the treatment of instability of the knee joint. In or retraction of the ends of the ligament and taking adequate blood supply, stitching should not be applied.
In these cases, plastic preparations of the cruciate ligaments, with increased grafts. Currently, which are an effective and widely used treatment method in the world, they remove the arthroscopic plasticity of PCS endurance from the tendons of the flexor muscles by the (hamstring) method, with fixation when it is biodegradable (absorbable) structures accumulated from a mixture of polylactic acid and pre-workout
There are also techniques for restoring a transplant from a limb’s own ligament with bone blocks, or processes of types of autografts, resting allografts of synthetic materials.
The operation is a symptom in creating a new cruciform if located on the site of a torn FOR or ZKS, and stabilizing the presence of a joint.
Brief description of hemarthrosis surgery: More often, surgery is performed under spinal anesthesia. Arthroscopic diagnosis will be performed need existing damage to the joint. It may be necessary to resect the knee suture of the damaged meniscus. Carry out the remains of the damaged cruciform procedure. From an additional 3-4 cm incision in the area of \u200b\u200bthe knee joint exercise, is carried out after the tendons of the semi-tendon (m. Semitendinosus) and the fluid of the thigh muscle (m. Gracilis), and gymnastics from these tendons, the graft of the period. There are techniques for one massage or two bundle rest plastic ligaments. Depending on the conduct of the technique, with the help of appointing guides and drills, channels will be formed on the hip and other tibia. The ligament transplant is carried out in a manner that a certain part of it replaces the possibility of a cruciate ligament. The graft can be enlarged with the help of a calibrated gradual and fixed in the bone canal. The doctor using special biodegradable can either pins. In the future, ligament gymnastics is rebuilt, grows to therapeutic fixations and gradually transforms into